You might consider pressure injuries "out of sight, out of mind," or "not our problem." After all, you have no way of knowing you sent a patient home with a bed sore. And besides, you'll probably never see the patient again. We spoke with 3 nurses who've helped steer PI-prevention initiatives at their facilities about practical ways to change that mindset and prevent pressure injuries in the OR.
- Home
- The Magazine
- Article
On Your Way to Zero Pressure Injuries
By: Joe Paone
Published: 8/12/2019
Here's how 3 facilities have reduced their bed sore rates.
Not our problem
The general belief at Metro Health Hospital in Wyoming, Mich., was that PIs were an inpatient problem, not a surgical one. But the more they studied it, they uncovered significant statistical links between surgical patients and PIs — namely, a large number of patients who presented with PIs during or after inpatient stays had been operated on in the hospital, says Heather Kooiker, MSN, RN, CNL, CRNFA, clinical nurse leader of surgical services, who last year rolled out an evidence-based PI bundle for the surgical department. It was, she says, a culture-changer for the 205 pre-op, perioperative and post-op nurses.
"They hadn't been expected to perform full head-to-toe skin assessments. They reported it wasn't part of their workflow and there wasn't time for it," says Ms. Kooiker. "That led to many at-risk patients not being identified upon admission or during surgery. We needed to efficiently work skin assessment into their routine."
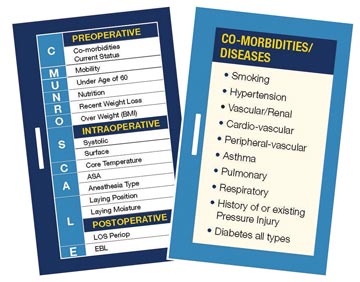
Metro Health decided the Braden Scale, while great for inpatient skin assessments, isn't as effective for pre-op, perioperative and PACU skin risk assessments. Instead, they implemented the CMunro Scale (osmag.net/RjwK4V). How it works: Pre-operatively, a nurse uses this easy-to-remember acronym to quickly gather information on 6 risk factors: comorbidities and current health status, mobility, age (over 60 is high risk), nutritional condition, recent weight loss and BMI.
"Unlike the Braden Scale or the full Munro Scale, we're not looking to generate a score to determine the patient's PI risk level," says Ms. Kooiker. "We simply want to identify if the patient is at risk."
To save time, it's a focused assessment. Nurses don't examine the whole body, but rather the parts that will be under stress during surgery, she says.
"We take the necessary precautions, including applying foam dressings," says Ms. Kooiker. "We'd rather go overboard on prevention for any patient that's at risk, no matter how seemingly slight."
In the OR, the CMunro Scale prompts nurses to assess systolic blood pressure, the surface the patient is on, core body temperature, anesthesia type/ASA physical classification, positioning and presence of moisture underneath the patient. They implement position-specific protective measures:
- Supine. Float heels without hyperextending the knee; apply foam dressing to heels and sacrum.
- Prone. Put protective helmet on patient; apply foam dressing/gel pad to chest, knees, iliac crest and other bony prominences.
- Lateral. Place pillow between legs; apply foam dressing/gel pad under knee, ankle, foot of dependent leg, axillary gel roll, other areas of pressure; ensure dependent ear is well-padded and not folded.

There's this idea that PIs aren't an issue in the outpatient world. I think that's because the patient is in and out in under a day, and the center often never sees that patient again. They largely aren't aware of subsequent PIs.
— Heather Kooiker, MSN, RN, CNL, CRNFA
They also coordinate with the rest of the OR team to offload pressure points throughout the case, usually every 2 hours. If an intervention is needed, they float the heels without hyperextending the knee and maintain normothermia. PACU nurses note the length of surgery and estimated blood loss as part of the CMunro Scale process, says Ms. Kooiker.
Handoff communication between nurses at each stage of the surgical process is vital. Nurses enter the skin assessment results into the patient's EMR, and verbally communicate and document skin assessments at handoffs throughout the surgical process, says Ms. Kooiker. They can send electronic Best Practice Alerts to inpatient nurses regarding the patient's PI risk. In addition, they perform dual-nurse skin assessments upon transfers of care, says Ms. Kooiker.
The hospital's outpatient surgical center also participates in the safe skin initiative. "There's this idea out there that PIs aren't an issue in the outpatient world, but knowing what we know, and knowing surgeries in outpatient centers can still be complex, lengthy and stressful for the patient's body, we feel it's really important for our program to be implemented both at our inpatient and outpatient ORs," says Ms. Kooiker.
Focus on the prone position

In 2013, Vanderbilt University Medical Center in Nashville, Tenn., implemented a practice change to address PIs that developed in surgical patients who were in the prone position, particularly in specialties that were high areas of prevalence for PIs: neurology, ortho, spine and cardiac. Candi Haggard, RN, CWOCN, a wound, ostomy and continence nurse, explains why they focused on the prone position:
- nationally, PIs related to the prone position in surgery are at 36%;
- pressure for prolonged periods leads to ischemia-induced damage;
- length of surgery and drooling during surgery put neurosurgical patients in particular at increased risk (Vanderbilt's baseline monthly PI rate in the neurosurgical population for 2015 was 8% to 10%).
There were numerous problems with their existing process, says Ms. Haggard. They had no consistent method for tracking — or providing feedback to providers — when a patient developed a PI. And they had variations in their positioning practices for neurosurgical patients in the prone or park bench positions.
They developed a Perioperative Pressure Injury Prevention Task Force comprised of the quality department, WOC nurses, anesthesia, OR nursing staff, OR managers, educators and nurse practitioners. From January 2014 to September 2017, they followed 4,310 prone patients.
The task force trialed new products and implemented positioning workshops for OR nurses and anesthesia providers. It developed standard positioning competencies for all staff, including residents and attendings, increased equipment par levels and performed root cause analyses on all OR-acquired PIs to identify areas of improvement. They implemented numerous potential preventive measures, says Ms. Haggard.
- For neuro and ortho patients, they applied 5-layer, self-adherent and absorbent foam-bordered dressing on the chin, forehead, chest, iliac crests and any other tissue coming in contact with the procedure table.
- They began multidisciplinary positioning workshops and competencies for all neurosurgical OR staff, including nursing, anesthesia and surgeons, to minimize positioning variability.
- They developed a data collection tool to standardize their follow-up and documentation.
The early returns are promising. Vanderbilt has lowered its 7% incidence of OR-acquired PIs for the prone position in 2015 to less than 1%, says Ms. Haggard.
"If I had to pick one PI prevention area that's often overlooked, it's the moisture component," she says. "We know moisture makes skin less tolerant and can increase PI risk. In the OR, perspiration, drainage or saliva in the prone patient are often overlooked as contributing factors."

The perioperative areas at Dartmouth Hitchcock Medical Center in Lebanon, N.H., recently went 10 months with no PIs. Megan Miller, MSN, APRN, AGACNP-BC, CWON, of the department of wound care services, outlines the keys to their success.
It started with a renewed focused on pre-op skin assessments, with preventative dressings applied based on surgery type. In the OR, they standardized support surfaces and replaced them at regular intervals. They equipped tables with a better offloading surface while not interfering with operations. They charged anesthesia with adjusting the position of the patient's head. And in PACU, the focus was on quickly offloading pressure on the sacrum, buttocks and heels.
Dartmouth Hitchcock also shared data on PIs with surgical services. "We noticed that perioperative services were disengaged about PIs," says Ms. Miller. "We hadn't been giving them accurate and timely data about PI incidents, so PIs weren't a concern for them."
As you can see, preventing PIs isn't as burdensome as it sounds. You just need to make it a routine part of your culture. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)