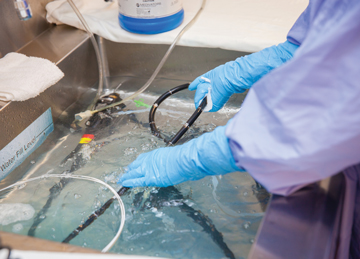
JUST CHECKING Small-diameter borescopes are one way to check lumens for residual bacteria after high-level disinfection. | Penn State Milton S. Hershey Medical Center
You might have expected the spread of the coronavirus to require altering your scope cleaning and HLD protocols in some way. Professional societies have recommended some minor changes (see "Proper Endoscope Care During the Pandemic" on
the previous page), but for the most part, COVID-19 simply
serves as a very loud wakeup call for you to revisit proper manual cleaning and HLD techniques, and reeducate your reprocessing techs on the importance of following the multiple steps involved in the processes.
With that in mind, make sure you have, and that your staff fully understands, the specific IFUs for each type of scope in your fleet. Are your IFUs up to date? Are all of the cleaning and care steps being followed?
Dr. Lim suggests checking in with your scope vendor, if you haven't already, to find out if the IFUs for your fleet of scopes have been updated since the COVID-19 outbreak. His vendor reported that COVID-19 doesn't require any changes to its scopes'
cleaning regimen. "I talked to them directly about it," says Lim. "Their stance is, as long as you follow what you're supposed to do, there should be no problem. What they publicly say, and what their data says, is that as long as you're cleaning
scopes the way they tell you to do it, there's no risk of transmission."
None of Dr. Lim's patients have turned up positive or transmitted the virus while in his care. "But we're currently performing procedures only on COVID-negative patients. At this point, I would be really reluctant to accept a COVID-positive patient
for an elective endoscopy." OSM
.svg?sfvrsn=be606e78_3)

.svg?sfvrsn=56b2f850_5)