Six Surface Disinfection Concepts
The puzzle of superior surface disinfection is never solved....
This website uses cookies. to enhance your browsing experience, serve personalized ads or content, and analyze our traffic. By clicking “Accept & Close”, you consent to our use of cookies. Read our Privacy Policy to learn more.
By: Daniel Cook
Published: 3/19/2020
John Hovanesian, MD, an ophthalmologist at Harvard Eye Associates in Laguna Hills, Calif., sends all his cataract patients opened-ended survey questions, asking them to share both the positives and negatives of their surgical experience. Unprompted, most patients complain about the difficulty of complying with the three-drop regimen — consisting of an antibiotic, steroid and NSAID — they're prescribed to improve post-op healing.
Eyedrops remain the most common form of medication delivery but that doesn't mean they provide the most benefit to patients, who often struggle to complete prescribed regimens. "Confusion is more of an issue than compliance," says Richard Hoffman, MD, clinical associate professor of ophthalmology at the Casey Eye Institute of Oregon Health and Science University in Portland. "We instruct patients to apply post-op drops four times a day until their follow-up visit, and direct them to stop only the antibiotic drops after day five. Some patients have instead stopped applying all of the drops by the time they come to the clinic."
The movement toward dropless cataract surgery continues. "It's exciting to see industry understand that post-op drop regimens are a problem that needs to be solved and is taking steps to develop solutions that reduce or even eliminate the number of drops patients need to administer after surgery," says Dr. Hovanesian.
Two sustained-release formulations hold the promise of eliminating the need for patients to apply a topical steroid.
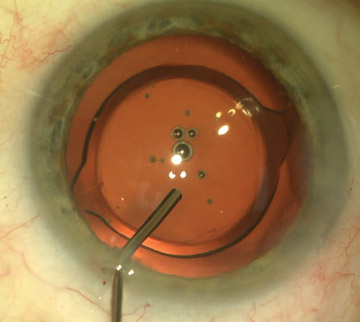
Dexamethasone intraocular suspension is administered into the ciliary sulcus at the end of cataract surgery after the viscoelastic has been removed from the eye. Following injection, the steroid suspension becomes a white liquid sphere in the anterior chamber and slowly dissolves to deliver a steady dose over the course of a month. The suspension has a good safety profile and doesn't increase the risk of intraocular pressure spikes when compared with topical dexamethasone, according to Dr. Hovanesian.
Surgeons can also opt for a preservative-free corticosteroid intracanalicular hydrogel insert that's placed through the punctum in the lower eyelid at the end of surgery, where it dissolves to deliver dexamethasone across the eye's surface for a month.
Topical antibiotics have never been proven to prevent post-op infection, but several studies have shown intracameral antibiotics are the most effective way to prevent endophthalmitis, according to Dr. Hovanesian.
He says it costs between $8 and $10 to buy a compounded moxifloxacin suspension that can be injected into the eye at the end of surgery. Surgeons can combine the suspension with one of the sustained-release steroids or a phenylephrine and ketorolac intraocular solution, which delivers a high dose of a nonsteroidal.
"The anti-inflammatory and anti-microbial regimen avoids eyedrops altogether for most patients who are not at high risk for cystoid macular edema," says Dr. Hovanesian. "In fact, I'm doing this in my practice with good outcomes. It's exciting."
Some surgeons are interested in eliminating or at least reducing the use of post-op steroids. Dr. Hovanesian injects a combination antibiotic and steroid behind the lens implant and into the anterior vitreous cavity, either through the zonules or through a pars plana. The injections essentially eliminate the need for patients to apply post-op drops. They aren't very expensive — ?$20 to $25 per case — and are a good option for patients who are unlikely to comply with a post-op drop regimen.
Ocular surface toxicity is often caused by topical medications, including steroids, because of the varying amounts of preservatives contained in generic preparations. "When we see patients three or four weeks after surgery, they're often frustrated that their vision is blurrier than it was a few days after surgery," says Dr. Hovanesian.
The sustained-release steroids eliminate this issue. "Both are free of preservatives and both provide a slow release into the eye," says Dr. Hovanesian. "There have been no significant incidences of intraocular pressure spikes."
Administering a combination of moxifloxacin and triamcinolone in an intracameral injection works approximately 90% of the time to prevent postoperative ocular inflammation and endophthalmitis, and eliminates the need to prescribe antibiotic and steroid drops, according to Dr. Hoffman. He says 10% patients who receive the injection might experience inflammation and require topical steroids or NSAIDs.
Dr. Hoffman is likely to use a subconjunctival steroid injection such as triamcinolone in patients at high risk for endophthalmitis if he's confident they aren't a steroid responder. He says a compounded combination of dexamethasone, moxifloxacin and ketorolac delivered intracamerally is a cost-effective option — approximately $25 per case. In comparison, a branded nonsteroidal and fourth generation fluoroquinolone could cost upwards of $300.
Administering intracameral injections at the time of surgery eliminates the need for physicians to call in post-op prescriptions and the treatment is also more convenient for patients, who don't have to venture out to pharmacies to pick up prescriptions. "It's pretty appealing — there are no worries about compliance and you remove a burden of care for patients, says Dr. Hovanesian.
It's exciting to see industry understand that post-op drop regimens are a problem that needs to be solved.
— John Hovanesian, MD
Surgeons can opt to prescribe a combination of prednisolone acetate, moxifloxacin and bromfenac in a single bottle, eliminating the need for patients to administer several drops daily. Dr. Hoffman prescribes patients prednisone, nonsteroidal anti-inflammatory drugs and antibiotics in a combination drop, whenever possible.
A recent study compared the outcomes of a standard three-drop regimen with a combination drop containing gatifloxacin, bromfenac and prednisolone acetate. Clinical outcomes were similar in both patient groups. Both groups experienced burning sensation after surgery, but patients who received the combo drop regimen felt less stinging than the patients who received the standard treatment.
A loteprednol etabonate topical corticosteroid that provides the benefit of a potent steroid without the associated side effects is indicated for twice daily administration, less frequent than the standard four-times daily dosing steroid regimen.
Dr. Hoffman says there is no significant risk in obtaining topical drops from a compounding pharmacy, but purchasing injectable medications is a bit more concerning. Make sure you partner with a certified 503B compounder, a designation that ensures it follows stringent quality control measures. Ordering compounded medications from a reputable company provides the peace of mind that you're receiving exact formulations of specific medications. OSM
The puzzle of superior surface disinfection is never solved....
Boston Children’s Hospital is renowned for its exemplary care on many fronts, including surgery....
Manual cleaning done properly is effective for eradicating microorganisms....