Six Surface Disinfection Concepts
The puzzle of superior surface disinfection is never solved....
This website uses cookies. to enhance your browsing experience, serve personalized ads or content, and analyze our traffic. By clicking “Accept & Close”, you consent to our use of cookies. Read our Privacy Policy to learn more.
By: Edwin P. Su, MD
Published: 10/14/2021
Many surgeons put very little forethought into wound care. The thought process is that when the procedure ends, the important work is done, so dealing with closing the incision is often left to assistants on the surgical team.
This is a mistake. Closing incisions properly is a critical part of the procedure. The wound is the access to the surgical site and should be considered a prime area that could permit the transmission of bacteria that could cause a surgical site infection. Delayed healing of the wound can compromise the results of the surgery. Fortunately, there are new developments in wound care that can help promote quick healing and limit the risk of potentially devastating SSIs.
• Negative pressure wound therapy. This innovation, commonly called wound vacs or incisional vacs, are vacuum-assisted dressings that have seen increasing usage in the last five years. They apply some negative pressure to the wound that stimulates healing. They’re extremely portable devices that patients can carry around with them as they live their lives and do their rehab. They essentially suck out excess fluid for about a week after procedures and contain the fluid in a chamber that doesn’t need to be changed. The method assists in healing and protects the wound during that critical period. The appropriate indications for these devices are high-risk patients, including those with high BMIs or people who have had multiple previous incisions. These portable vacs have proven to be very helpful for these patients.
The units can be clipped onto patients’ pants or held in a carrying case that has adjustable straps. The wound is dressed with a water-resistant cover and the patient can shower with the doctor’s permission. The device applies negative pressure to the dressing and a tube connects the dressing to the canister where the fluid from the incision is collected. The device is worn for about seven days. Some models come with a rechargeable battery and a charger. It’s a good idea to tell patients to charge the batteries while they’re sleeping to reduce the possibility of the device running out of power while they’re out of the house for an extended period.
In addition to removing fluid from the incision site, the devices aid recoveries by protecting the wound from outside sources of infection and assisting in holding the edges of the incisions together until they fully heal.
The devices are worn around the clock, except when showering. The dressing should never be submersed in water, and direct water spray from the shower shouldn’t hit the dressing. Before showering, the device should be turned off, disconnected from the dressing, and the clamp on the tub should be closed. Patients should be instructed to not disrupt the dressing when using a towel to dry.

• Antibacterial dressings. More attention is being paid to dressing the wound, which is another positive development. Antibacterial dressings include sponges impregnated with silver (an antimicrobial) and are applied to patients in the sterile field, which is where surgeons can place the cleanest dressings on the wound. The absorbent silver-laden sponge can soak up and handle any fluids that leak from the wound.
These dressings are appropriate for all types of surgeries. They’re more expensive than dressings that are not impregnated with silver, but definitely worth it. Infections are disabling for patients, who would need an antibiotic regimen at a minimum. They’re also potentially very expensive to treat and to litigate. These dressings can always be taken off, but work best when they’re on during the first few days of recovery.
When patients or an aftercare team take off the initial dressing in 48 hours, check the wound, then cover it again, they’re exposing the wound before it’s totally sealed. I prefer to put the antibacterial dressing on immediately after the procedure and have it remain in place for seven to 10 days before the patient is instructed to change it. This is an effective practice because the wound is being protected during the critical healing time when it’s not yet watertight and therefore still susceptible to contamination.
Antimicrobial dressings are completely waterproof, so it’s fine for patients to shower with them on after they go home. I tell them to resist the temptation of opening them to peek at how the wound is healing. I impress upon them that, again, this is the cleanest dressing we can put on your wound, so it’s important to leave it on for a week to 10 days unless they really feel like something is wrong.
Some discoloration of the sponge is normal and not a cause for concern. If the drainage isn’t stopping within two or three days, if patients feel significant pain or there is some visible redness that seems to be spreading beyond the incision, they should call their doctor. In rare cases, some people might get some minor skin irritation, likely an allergic reaction to the adhesive, so the dressing could need to be removed in those cases.
• Subcuticular closure. Staples were the standard in closing skin incisions for a long time, but there has been a significant shift in the last few years toward newer options that do a better job of closing the wound. Subcuticular closures with some sort of thin skin adhesive such as glue create a watertight wound that I and most of my colleagues use. They’re very convenient: patients can generally shower right away with them in place, and there’s no need for a return visit to have staples removed.
These noninvasive adhesive wound-closure products can be economical because surgeons shave precious minutes at the end of a case when closing the wound, and those minutes add up to a more efficient and less expensive day in the OR.
Every staple represents potential entry points for bacteria, so SSI risks also go down with adhesives. Patient satisfaction is an additional benefit, as significant scar tissue can be a negative even for patients who go into surgery saying they don’t care about scarring.
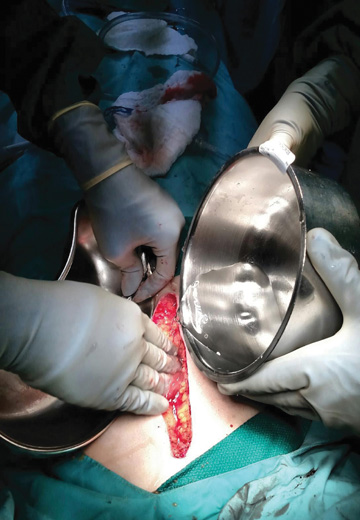
• Wound irrigation. Diluting the wound at the end of surgery with any number of irrigants remains an important component in the continuum of surgical care. Flushing the wound is vital because bacteria or debris could be present and must be removed. The process also rids the wound of nonviable tissue and exposes healthy tissue. If the bacteria and foreign debris is not flushed out, they could pool, which could create abscesses or infections.
Newer options to saline and betadine are more effective in destroying biofilm and aren’t toxic to bone tissues and skin cells that need to heal. Antiseptic agents and detergents can be used with high- or low-pressure lavage or a bulb-syringe lavage.
The exciting new developments in wound closure are appropriate for use in outpatient facilities, and can make treatment of surgical wounds less of an afterthought for surgeons who should give the practice the attention it deserves. OSM
The puzzle of superior surface disinfection is never solved....
Boston Children’s Hospital is renowned for its exemplary care on many fronts, including surgery....
Manual cleaning done properly is effective for eradicating microorganisms....