April 25, 2024
Growing demand for anesthesia services at ASCs is being met with a dwindling supply of anesthesia providers....
This website uses cookies. to enhance your browsing experience, serve personalized ads or content, and analyze our traffic. By clicking “Accept & Close”, you consent to our use of cookies. Read our Privacy Policy to learn more.
By: Jared Bilski | Managing Editor
Published: 8/3/2022
Surgeons are often compared to elite competitive athletes, but perhaps professional dancer is more appropriate — at least when it comes understanding the ergonomic and musculoskeletal issues physicians face throughout their careers. “When you think about a dance performance, you have to stress and strain every muscle for a prolonged period of time, often in a frozen position, and that high-muscle tension can cause the types of injuries far too many surgeons encounter throughout their careers,” says Scott T. Hollenbeck, MD, a plastic and reconstructive surgeon at Duke University Health System in Durham, N.C.
The wear and tear of the repetitive surgical motions and the awkward positions in which physicians tend to contort themselves to perform various procedures often result in serious and sometimes career-ending injuries. In fact, Dr. Hollenbeck says 30% to 70% of surgeons have had to shorten or modify their careers because of a musculoskeletal injury. These issues aren’t typically happening to surgeons who are at the tail end of their careers, either. “One of the most surprising things about these injuries is that they occur mainly to surgeons in the early- to mid-career level,” says Dr. Hollenbeck. “It’s typically the type of injury that surgeons in their 40s and early 50s develop because that’s the busiest and most productive point in their career, and they’re working hard and generally doing more difficult cases.”
Luckily for Dr. Hollenbeck, the health system in which he works understands the critical role proper ergonomics plays in preventing musculoskeletal injuries, extending surgeons’ careers and increasing their job satisfaction. Duke Health recently rolled out an ergonomics program specifically for surgeons that was a collaboration with the Duke Ergonomics Division and its department of surgery. The main goal of the program is injury prevention. Unfortunately, preemptive efforts to prevent these types of problems aren’t always a realistic goal. “A lot of times, an injury has already occurred, so we work with departments and surgeons to address the ergonomic risk factors that may have led to musculoskeletal disorders,” says Marissa Pentico, MS, OT/L, CPE, ergonomics coordinator at Duke Health.
• Direct observations. Under the program, surgeons fill out a discomfort survey on the types of procedures that are causing them the most issues, which in turn gives Ms. Pentico and her team a good starting point to focus the direct observations they conduct of the surgeons in action. During the observations, members of the ergonomics team watch surgeons as they operate and take photos of what they see. “We’re looking for risk factors related to their postures, the positions in which they’re working, the duration with which they’re working in awkward positions and the frequency with which they’re doing it,” says Ms. Pentico.
Armed with photographic evidence of problematic postures and positioning, Ms. Pentico meets with surgeons to discuss injury mitigation strategies. As Dr. Hollenbeck will attest, this review session is often an eye-opener for the surgeons who weren’t aware of just how bad their postures are. “When Marissa shows you the pictures, you’re like, ‘Oh my god, that looks really bad,’” he says. That mental picture leaves an indelible mark, something that comes in handy when they find themselves in that same position during future procedures. “Later on, you’ll think, ‘OK, this is that risky part of the procedure, I’d better move through this or stop to take a break,’” says Dr. Hollenbeck.
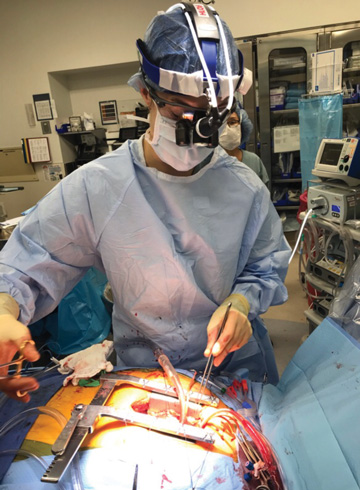
• Helpful advice. Recognizing potential problems in real-time is one of the best ways to prevent future injuries, and these observation sessions have had a dramatic impact on the awareness Duke surgeons have of proper positioning — as have the loupe-fitting changes that are part of the surgeon ergonomics program. Poorly fitted loupes that surgeons use to magnify and visualize the surgical field can cause them to bend their necks at awkward, uncomfortable angles during surgeries, which often leads to strain injuries.
To remedy this common issue, Duke Health made some major changes to its loupe-fitting practices with the aim of helping the next generation of surgeons. To ensure interns are better educated on the proper way to wear loupes, residents were brought in to consult with them prior to their fittings. “The residents guide the interns on what to look for in a fitting and how the loupes should fit, and that’s been really helpful because interns have been basing their decisions solely on what the vendors told them,” says Ms. Pentico.
Interns are also given an opportunity to make modifications if they’re having problems with their loupes. “Within three months, the expectation is that interns will have a follow-up session with the vendor if they need to change the fit,” says Ms. Pentico. “Vendors know they must be available to make the changes within that time frame.”
The location of the fittings has also undergone an overhaul, moving to a SIM lab with a height adjustable table, a training mannequin and suturing kits. The change, says Ms. Pentico, ensures interns are being fitted while they’re performing a suturing task at a table height that they indicate is in line with what they typically use in the OR. The emphasis on proper fitting is crucial because of how long physicians spend with the equipment. “We have attendings who have been wearing the same loupes for 15 to 16 years, so we need to get our interns started off right,” says Ms. Pentico.
• Regular breaks. Even if your facility doesn’t have the resources to invest in a formal ergonomics program, there are plenty of things your staff can do to protect themselves from injuries. Dr. Hollenbeck swears by regularly stretching and performing exercises that are geared toward straightening muscles around the spine and flexing or extending his body back into more of an upright position. “Surgical team members are often bending over and forward in order to see down into the patient during surgery, so they want to stretch the postural muscles in the back as opposed to the abdominal muscles,” he says.
Dr. Hollenbeck has also incorporated microbreaks into his surgical routine, short resets or stretches that occur every hour during longer cases. “Microbreaks let the team pause and perform the postural muscle exercises and activate muscles in the neck,” he says.
If you work at a high-volume outpatient facility that strings together a series of shorter cases, Dr. Hollenbeck suggests dedicating some portion of the OR turnover time to limbering up and repositioning your body in a better way, even if it’s just standing with your back against the wall and stretching out your arms.
One of the most important factors impacting proper ergonomics in the OR is the culture shift that is occurring right now. In the past, says Dr. Hollenbeck, surgical professionals didn’t talk much about ergonomics, proactive stretching and preventing musculoskeletal injuries because they feared that admitting they were hurt or injured would impact opportunities to advance their careers. “Injuries weren’t discussed because people used to think that if you wanted to be a surgeon, you had to accept that your body was going to pay for it,” says Dr. Hollenbeck.
Now organizations like Duke are shining a light on just how outdated and problematic the push-through-the-pain mentality truly is for surgeons, and it’s up to facility leaders to make proper ergonomics a priority in practice. OSM
Growing demand for anesthesia services at ASCs is being met with a dwindling supply of anesthesia providers....
Improvements in both workflow and staff attitudes are part of a leader’s responsibilities, but your interventions in these areas don’t need to be major to make...
The ASC market continues its rapid growth. In 2023, roughly 116 new ASCs opened in the U.S., many of which were orthopedic-specific in nature....