- Home
- Article
10 Proven Slip-and-Trip Prevention Tactics
By: Jennifer Parrott, RN
Published: 6/25/2024
These practices will put you on the path to a near-perfect safety record.
A safety-first culture in your operating room includes protecting the staff as well as the patients. We haven’t had a fall in nearly a decade because keeping members of our OR team upright is a top priority. Here are 10 ways to reduce or eliminate slips, trips and falls:
1. Dial it back a notch. Slow down. Don’t move too fast. You’ve got to make the safety last. These phrases serve as important reminders of what matters most.
We strive for turnover times between three to 16 minutes depending on the case, but staff safety is the most important metric. It’s important to regularly remind your team their welfare comes first.
2. Traffic control. We aim to keep as much equipment as possible along perimeters of the room until needed, so it’s not in the main area of foot traffic. We also use our anterooms to hold extra equipment and non-sterile supplies that might be called for throughout the day to keep the ORs free of nonessential clutter. Additionally, we direct as much foot traffic as we can through our sub-sterile rooms to keep air disturbance to a minimum.
3. Manage cords and cables. When going wireless isn’t an option, we place all machines with cords toward the back of the room. This minimizes the length of cords on the floors. The sections that are in the open are safely secured with cord covers.
Always be aware, however, that even cord covers are potential trip hazards. Though much safer than exposed cords, covers still can be turned upside down by the foot of a staff member. This is why we keep the lengths of cords on the floor to a minimum.
Our OR teams are also asked to wear closed-toe, slip-resistant shoes, which help with infection control and protect them from tripping.
4. Lighting types and outlet placement. Fluorescent lighting is preferable because its brightness allows everyone in the room to see clearly and identify if there are any hazards in the way. We also try to use outlets on our ceiling-mounted booms and towers, or ones that are at the head of the room where the anesthesia machine is located to reduce cord clutter. We try to not use the outlets located elsewhere in the OR for devices that would require a cord on the floor.
Reeducation and declaring a people-first culture is the best way to minimize slips, trips and falls.
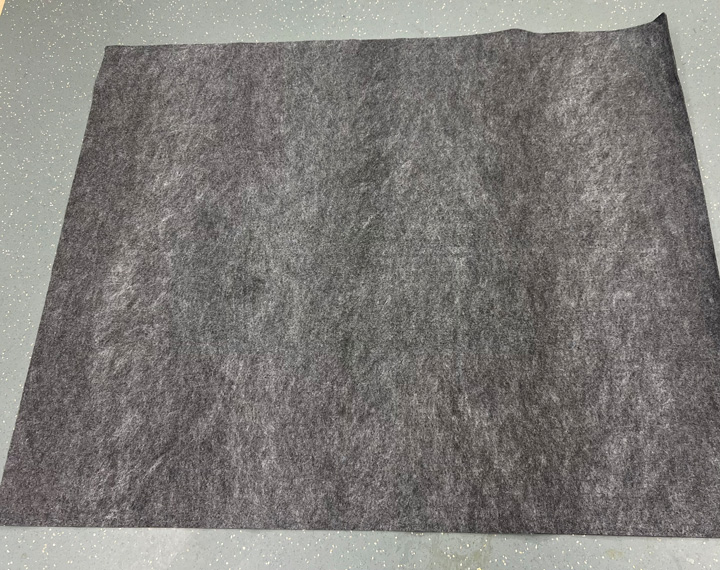
5. The fluid situation. We use black mats that are very absorbent during arthroscopic procedures — as many as are needed. Generally, however, only one or two are required to absorb the splash-off. The mats, which have a slip-resistant backing, are simply rolled up and disposed of at the end of each case. We also use an aspirator with small plastic attachments that we put on the floor to suck up fluids not absorbed by the mats.
6. Cleaning the floor. This is the last task of the room turnover. We use a cleaner/disinfectant with a short drying time — around three minutes. Using products that take several minutes to dry increases the chance of someone falling. Our flooring has a slightly textured surface that’s designed to reduce fall risks even when it’s damp.
7. Surgical checklist. We always go over any special equipment needs and other concerns during the time out. This gives the staff a chance to reconsider where they’ve placed items in the room and think about changing things if necessary. The surgical safety checklist contains a fall risk assessment to address any heightened concerns about the case at hand.

Nearly half of the 1,411 sentinel events reported to The Joint Commission (TJC) last year were falls, according to the agency’s annual report on the occurrences that cause significant harm that was released in May.
Patient falls have been the leading type of sentinel event reported to TJC since at least 2019. A total of 672 events categorized as patient falls were reported in 2023, nearly 48% of all reported events. The main types of injuries suffered during the falls were broken hips, legs, shoulders, arms or ribs, as well as head injuries. Approximately 4% of the falls were fatal, 8% resulted in permanent harm to the patient and 80% caused severe harm, according to the report.
Thirty-five percent of the falls took place while the patients were ambulating, 25% of the cases were patients falling from beds and 19% occurred while patients were toileting. The report states a mix of not following fall risk assessments, inadequate ability to recognize abnormal clinical signs or signals, and poor staff-to-staff communication during handoffs or transitions of care contributed to the incidents.
Wrong surgeries were the second most frequent sentinel events last year, making up 8% of the events reported. The TJC has resources such as this one to help guide facilities in reducing patient falls.
—Outpatient Surgery Editors
8. Staff training. In small OR spaces where people are moving quickly, situational awareness is critical. All team members must be cognizant of their surroundings and how the actions of their teammates could impact them. We train everyone on what to look for in advance, so they’re prepared to act when they open the door with no surprises. Also, immediate training should be conducted when a new product that has a cord arrives. This shouldn’t be delayed until annual safety measures are reviewed. We’re vigilant about training new employees on safety issues and require existing employees to maintain a safety competency.
9. Fight fatigue with culture. To truly make safety a priority, it’s important to place a high value on keeping the team sharp. Despite constant pressures at high-volume facilities to get the job done, the culture must encourage staff to speak up if they need a break during their shift or if they require a mental health day.
10. Eternal vigilance. Reeducation and declaring a people-first culture is the best way to minimize slips, trips and falls. There’s no surefire way to completely prevent them, but when an incident does occur, we investigate immediately, identify what went wrong and take measures to prevent it from happening again.
An initiative-taking approach is a must. Taking these risks lightly puts staff at risk. Prevention processes should always be a top priority. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)