It was early on during the launch of our facility's orthopedic program when we recognized the importance of relying on regional anesthesia to ensure patients go home sooner, recover more effectively and experience less pain and nausea.
About a decade ago, a group of our surgeons, anesthesia providers, nurses and physical therapists collaborated on how to best manage the pain of orthopedic patients. We created a nurse-led team that makes sure nerve blocks are administered consistently, safely and efficiently.
The block program has been a boon. Surgeons prescribe fewer opioids to manage post-op pain and patients who have had previous surgeries without regional anesthesia are often astounded at the difference a nerve block makes. The number of patients who request blocks and the number of blocks we place have increased each year, and we're now looking to expand their use beyond orthopedic patients to general abdominal, gynecological and breast surgeries. We've learned that a multimodal pain management plan will improve orthopedic outcomes and increase patient satisfaction if it's built on these 5 pillars of nerve block success.
1. Facility-wide buy-in
To make a regional anesthesia program work, be as inclusive as possible of all the staff across the many disciplines who are involved, including, nurses, anesthesia providers and surgeons. You need to create a united, team atmosphere.
Your surgeons might push back against your efforts to standardize the block-placing process in a dedicated procedure room, preferring instead to place the blocks in the OR. They might even want to avoid blocks altogether, thinking the time it takes to place blocks will delay the start of their cases. That's OK. A very important part of establishing a successful block program is to acknowledge and address each surgeon's concerns, preferences and needs. Assure them that a well-run block program can actually increase overall surgical efficiencies.
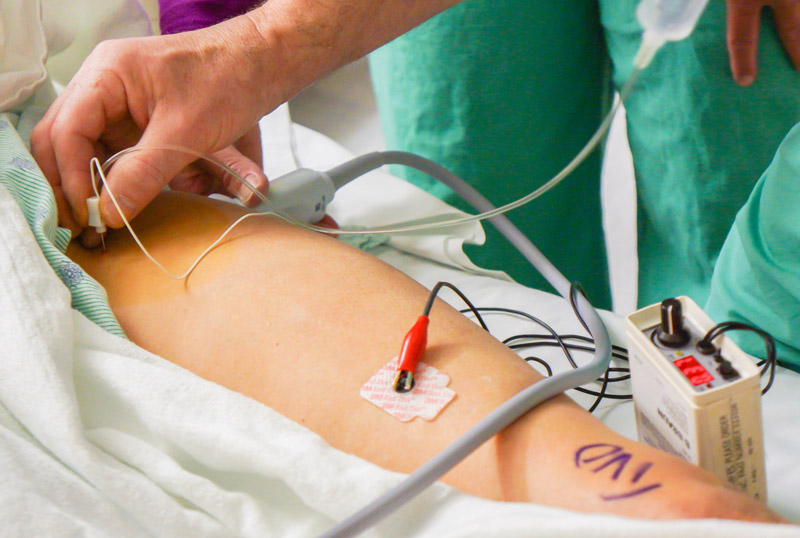
Our nurses are trained on how to use ultrasound machines, nerve stimulators and other equipment needed to place blocks. They also have significant training in pain management, and acquire competencies in administering sedation.
The importance of maintaining patient safety, particularly after a nerve block, is one of our prime concerns. Communication — through verbal handoffs and charting regarding the blocks performed — ensures continuity of care, as nurses and staff are aware of mobility and weight-bearing concerns. Physical therapists tailor their post-op rehab program for each patient based on the type of block performed.
The number and types of blocks we perform change over time related to increased knowledge, research and newly identified best practices.
2. Pre-op planning
Begin preparing for block placement a couple days before surgery, when you're reviewing the surgical schedule. The selection of nerve blocks performed are individualized to each practitioner and patient, based on the surgeon's technique and the patient's unique medical history. When a surgeon books a case, we look at the surgeon's preferences and the patient's health history to determine which nerve block will be most effective, and what kind of needles and supplies will be needed. This advanced information and planning reduces delays in surgical start times. We also worked with our team of anesthesiologists to standardize the local anesthetic they administer and the supplies they use. Because so much of the process has been standardized, our team is very efficient in preparing the sterile field for the anesthesiologist who will administer the blocks.
3. Keeping patients informed
Educating patients about how blocks are placed and keeping them informed throughout the process are important elements of a successful regional anesthesia program, because it can be a little disconcerting and frightening to be told you're going to get a nerve block. Patients often say they feel overwhelmed and rushed into making decisions, with mass amounts of information being given in the short amount of time before surgery. The more information you provide ahead of time, when the patient is less apprehensive, the more the patient will be able to understand and participate in their pain management plan. Giving patients time to verbalize questions or concerns is also key to ensuring they have a good surgical experience.
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)