Adding new and innovative procedures is a proven way to increase your revenue, attract new patients and surgeons, and set yourself apart from the competition. And yes, total joints is all the rage right now, but it's far from the only way you can expand your offerings. Here are 5 other well-paying, satisfaction-bolstering procedures that are relatively easily to add to your facility.
- Home
- Article
5 Procedures Worth Adding
By: Jared Bilski
Published: 7/18/2019
These surgeries are popular, pay well and are easy to incorporate.

1. Minimally invasive glaucoma stents. In 2016, the FDA approved Xen45 Gel Stent and the Xen Injector (osmag.net/dD7RrJ) for several groups of glaucoma patients, including those who suffer from the more common open angle variety of the potentially blinding disease. The Eye Surgery Center of Western Ohio in Lima recently added these stents to its list of available glaucoma treatment options. With this minimally invasive procedure, the surgeon implants a soft, permanent stent (approximately 6 mm long and as wide a human hair) through a small, self-sealing corneal incision. The stent shunts fluid from the anterior chamber of the eye to the subconjunctival space. The result is a reduction in both intraocular pressure and the need for irritating, allergy-inducing and expensive eye drops — a real patient satisfier. Plus, the stent procedure takes much less time than a trabeculoplasty, the more common and time-consuming treatment for this type of glaucoma. The stents, which run $1,450, can be inserted as a stand-alone procedure or in conjunction with a cataract surgery, and they're reimbursed by CMS.
"This procedure is generally reimbursed well by CMS, but you'll want to keep in mind it's billed through a temporary code," says Diane Repko, RN, nurse director of the Eye Surgery Center of Western Ohio. "That means you'll want to do your homework — always pre-authorize and be prepared to jump through the hoops some payers make you jump through to get paid using temporary codes."
Temporary codes (CPT Category III) represent emergent or experimental services, technology and procedures, and are used for data collection purposes to support widespread usage or to provide documentation for the FDA approval process.
Beside the implants, eye centers generally have everything they need in place to conduct these procedures. But like much new OR technology, you'll have to rely heavily on your sales rep to talk you through the finer points of the implant. "Reps tend to focus solely on the physician and ignore nurses and techs, which is frustrating," say Ms. Repko. Whenever possible, ask your sales rep to speak to the entire clinical staff outside of the OR to answer questions or concerns about the new procedure, she adds. When it comes to scheduling, you may want to wait for the end of the day to do these procedures — at least initially.
"We do a lot of straight-up cataracts, and we don't want to bottleneck ourselves with delays early on, so we do all our Xen's (stents) at the end of the day," says Ms. Repko. The instrumentation takes about 10 to 15 minutes to set up and the procedure itself takes 10 to 15 minutes, depending on the surgeon, adds Ms. Repko.

2. Spinal stimulator implants. If you want to try your hand at minimally invasive spine procedures, you might want to follow in the footsteps of Gadsden (Ala.) Surgery Center. The ASC recently began performing spinal cord stimulators (SCSs) — also known as dorsal column stimulators (DCSs) — as a pain management option for patients with chronic back pain. In a nutshell, the SCS procedure involves an implantable neuromodulation device that sends mild electrical signals to select areas of the spinal cord to reduce pain.
"When CMS announced it was reimbursing the stimulator implant, we decided it was a good opportunity for us to move into spine procedures," says Harriet Willoughby, RN, BSN, Gadsden's CEO. Indeed, CMS just started reimbursing for this procedure in 2018, which is a major incentive when you consider the stimulator implant itself costs $25,000.
And the implant isn't the only high-ticket item associated with this procedure. If you're not already outfitted for spine, instrumentation is a significant investment. You'll need a Jackson table with a Wilson frame, a cooling vest, a basic laminectomy tray and at least 2 electrocautery machines, says Pat Daniel, RN, the manager at Gadsden Surgery Center. From a staff perspective, Gadsden conducts the approximately hour-long procedure (not including the 20 to 30 minutes of prone positioning) with both a physician and PA in addition to 2 circulators, 2 OR techs, 1 X-ray tech or someone who's well-versed in fluoroscopy.
If you're considering this procedure at your facility, research is absolutely crucial. After all, you're dealing with some large upfront investments here.
"I was used to ortho cases with $500 to $1,000 implants, so when I saw the $25,000 price tag on the stimulator, I was sweating bullets on that first case," says Ms. Willoughby.
She ended up borrowing spine instrumentation from the local hospital to save on the upfront costs of her center's first SCS procedure.
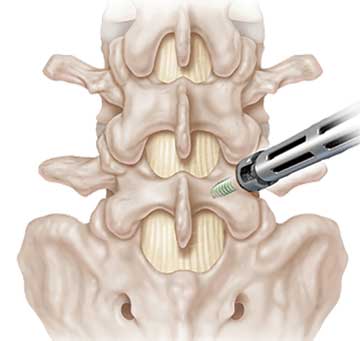
3. Minimally invasive TLIFs. If you've recently outfitted your facility for spine and are wondering what other procedures you can add to the menu, minimally invasive transforaminal lumbar interbody fusion (TLIF) may very well be right for you. The TLIF procedure is used to treat back or leg pain stemming from degenerative disc disease by fusing the anterior columns and posterior columns of the spine — via bone grafting, an interbody spacer, as well as pedicle screws and rods — through a posterior approach, which is done with smaller incisions, less disruption to muscle tissue and ultimately a quicker recovery than a traditional anterior fusion approach.
"This is the type of procedure that physicians increasingly want to do in an outpatient setting and that commercial insurances tend to pay very well for," says Marcia Van Alstine, RN, CNOR, CASC, the executive director at Semmes Murphey Surgery Center in Memphis, Tenn. But be forewarned: TLIFs are labor-intensive, time-consuming procedures that can take anywhere from 2 to 4 hours to perform, depending on the surgeon. Because of the time-intensive nature of the procedure, effective scheduling is key. As a general rule, you'll want to schedule TLIFs first thing in the morning and, even though this is a same-day procedure, prepare for the unlikely possibility that a patient may have to stay the night.
"We always make TLIFs the first case of the day, we only schedule 1 per day and we book every procedure 2 weeks in advance to allow for our nurses to sign up for overnight shifts (2 RNs are required in the event of an overnight stay)," says Ms. Van Alstine. While the extra preparation is a must, the vast majority of Semmes's TLIF patients walk out the doors of the surgery center by 6:30 or 7:00 p.m.
Again, unless you're already outfitted for MIS spine, this probably isn't the right procedure for your facility. At a minimum, your facility needs a Jackson table with a Wilson frame (surgery in prone position), a C-arm, a decent neuro microscope and a tubular retractor instrumentation. The latter was an easy one for Semmes because one of its physicians, Kevin T. Foley, MD, FAANS, invented a well-known tubular system: the METRx, a micro endoscopic discectomy system that features a series of sequential muscle dilation tubes. "So we were lucky in that we didn't have to buy anything extra there," says Ms. Van Alstine.
Medicare doesn't currently reimburse for the procedure, but commercial payers do (see "Medicare Reimbursement"). Be extra careful your coding team is billing everything correctly.
"Certain insurers will bundle the payment, so it's up to you to make sure CPT codes are included and the payment is going to cover everything — including the rare case of an overnight stay," says Ms. Van Alstine. "Remember, this is a new procedure so you may have to go back through your payer contracts and make sure everything is covered."

4. Total thyroidectomy. Some procedures aren't reimbursed by CMS, but still get great reimbursements from private payers in most cases. One such procedure is an outpatient total thyroidectomy, a minimally invasive surgery to remove a patient's entire thyroid. Such a procedure has become a high-volume staple at Ohio Surgery Center in Columbus, where 137 of these procedures were conducted last year alone.
Like any new surgical endeavor, you'll want to start slowly with this procedure because instrumentation could be pricey, and there may be some growing pains in terms of your scheduling. "You don't want to go guns blazing and buy 5 sets of instruments if you're just starting out and haven't done any cases," says Suzi Walton, the facility administrator at Ohio Surgery Center. "When we started, we couldn't do more than 2 thyroid cases per day. As we grew the program, we reinvested accordingly."
Speaking of instrumentation, you'll need a soft tissue tray and a thyroid tray, as well as a harmonic scalpel — a device that can simultaneously cut and cauterize tissue — for speed, as well as the ability to do same-day parathyroid hormone (PTH) testing on the patients. Schedule-wise, it can be tricky — especially if your physicians want an additional surgeon to serve as an assistant during the procedure. Your best bet: Schedule early, leave plenty of room for unforeseen complications and adjust as you get used to doing the thyroid procedures more efficiently.
"We scheduled all of our initial total thyroids first thing in the morning, or as early as possible, so our staff could sit on the patient longer in the PACU if need be," says Ms. Walton. The PACU, in particular, is an area where extra training is paramount. Your staff must be able to spot any potential complications. For example, if you need to change a patient's dressings (showing bright red) 5 times within an hour post-op, your PACU staff should get the surgeon back in to see what's going on.
From a financial perspective, this procedure presents a golden opportunity for facilities that can handle a high volume of total thyroidectomies. Reason: Commercial payers are putting pressure on providers to move this procedure to the outpatient setting whenever possible. In fact, one of Ohio Surgery Center's major payers was directly responsible for the facility's influx of total thyroid cases. The payer actually came to the surgeons in the facility's ENT group with data on what surgeons were doing what at the hospital and gave them an incentive to migrate a certain percentage of them to the surgery center. This need gives you some leverage. But if you're going to add this procedure at your facility, you need to do your homework, know your costs and negotiate heavily with your payers about carve outs in your contracts. "For us, reimbursement wasn't just X-percentage of Medicare," says Ms. Walton. "Our payers were very willing to work with me on costs and gave me really good reimbursements because they were still paying a third or even a fourth of what it costs to have these procedures done in a hospital."

5. Robotic hernia repair. It wouldn't be right to talk new procedures without mentioning robotics — and robotic hernia repair, inguinal hernias in particular, are increasingly being done on an outpatient basis. For good reason. Price, the ultimate barrier for most hospitals and ASCs, isn't quite as restrictive as it was just a few years ago. Granted, the $1 million to $2 million upfront cost and $100,000 annual maintenance costs make the robot seem out of reach for many facilities, but vendors now offer a number of manageable payment options.
"Companies have gotten smarter about financing. Facilities now have several programs to choose from," says Sharona Ross, MD, FACS, professor of surgery at the University of Central Florida (UCF), and director of minimally invasive surgery and surgical endoscopy at Advent Health Tampa. "You don't have to pay for everything up front."
Without factoring in the upfront investment, robotic inguinal hernia repairs are actually less expensive than traditional laparoscopic procedures because the latter requires surgeons to use several expensive disposables like balloon spacemakers and tackers, items you don't need with the robot. If you're a facility that can do a high volume of these procedures, the savings add up. But for the time-being, outpatient reimbursement for inguinal hernia repairs — Medicare reimburses in the $1,700 range for ASCs and most in-network insurers pay about the same — still don't cover the fixed costs. But as these procedures grow in popularity, that could easily change. Plus, it's hard to place a number on the marketing value robotic surgery adds to your facility.
| Procedure Type | CPT Code | ASC Reimbursement Rate | Hospital Reimbursement Rate |
|---|---|---|---|
| Xen gel stent for open angle glaucoma | 0449T | $2,636 | $3,640 |
| Spinal cord stimulator (SCS) | 63650 | $4,499 | $5,979 |
| Laparoscopic inguinal hernia repair | 49650 | $2,129 | $4,595 |
| TLIF | 22630 | Not currently reimbursed | Not currently reimbursed |
| Total thyroidectomy | 60220 | $2,129 | $4,595 |
If you do opt to go the robotic hernia repair route, efficiency is the name of the game. You should be able to do these cases quickly. A skilled team can dock a robot in 2 to 3 minutes, and an experienced surgeon should be able to do the surgery in 20 minutes. Overall, a robotic inguinal hernia repair shouldn't take more than a half hour, says Dr. Ross. The key word here is should. When you're starting out, there will always be inefficiencies and ways you can improve turnover time. The way to do it?
"Break down the procedure step by step," says Dr. Ross.
"Record how long it takes to get to the room, the time it takes to intubate the patient, and the time it takes to dock the robot, perform the surgery and close. When you break it down this way, you'll find ways to improve turnover." OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)