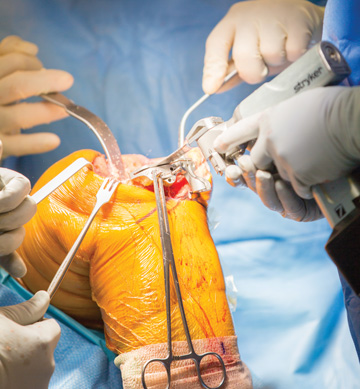
You can’t see them, but they’re there. Minute traces of airborne dust particles, skin cells and microbes are swirling around the sterile field, waiting to touch down on instruments, surfaces, implants and surgical wounds. Our research has shown that numerous bacteria move throughout the OR air, even in the presence of an adequate ventilation system (HVAC) with laminar flow. The amount of airborne particulate in the OR air is directly correlated to the number of people in the room during a case — it’s estimated that 30% of surgical team members are carriers of Staphylococcus aureus. When staff members move into and out of the OR during surgery, they interrupt laminar airflow, which increases the risk of airborne contaminants reaching the sterile field. Laminar flow is also disrupted when its currents hit stationary objects around the surgical table.
Current standards for OR air quality are based on engineering requirements for air flow and ventilation. They do not address specific evidence-based criteria for the quantitative reduction of viable microbial aerosols. So how do you measure and manage potentially infectious aerosols in the OR air?
There are no practical ways. Perhaps that’s why infection preventionists often focus on contact contamination, aseptic technique, the shedding of skin flora from surgical team members and patients, surface disinfection and hand hygiene in their efforts to reduce contamination risks in the OR.
That’s certainly understandable. But we now have access to sophisticated data that clearly show airborne contamination is occurring in the OR. There is also an increasing body of clinical evidence documenting that airborne microbial populations can contaminate the surgical wound and increase the risk of post-op infection, especially during joint replacement cases. Our own studies have shown that airborne gram-positive bacteria were present within 1 meter of the surgical wound in an OR with optimal laminar flow and regular air exchanges (osmag.net/N4hAZv). Numerous other studies have linked airborne contamination to orthopedic SSIs.
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)