Doing away with compounding in the OR will improve patient safety and case efficiencies. It will also make sure your facility complies with USP 797, which governs a wide range of factors that ensure compounded drugs are prepared in a dedicated space by specially trained pharmacists who follow strict quality controls and do all their mixing under a laminar air flow hood.
Perhaps you're looking to stop compounding in the OR, but feel overwhelmed at the prospect of overhauling a practice that's become a cornerstone of your day-to-day procedures. Sure, you can outsource anything you mix in-house to a compounding pharmacy (see "5 Questions to Ask Your Compounding Pharmacist"). But if your facility has safety or cost concerns, or simply doesn't have the time or resources to properly vet an outside compounder, there's another option. You can start small by focusing on a specific medication or solution you want to stop mixing in the OR and break down the process step by step until you find a better way.
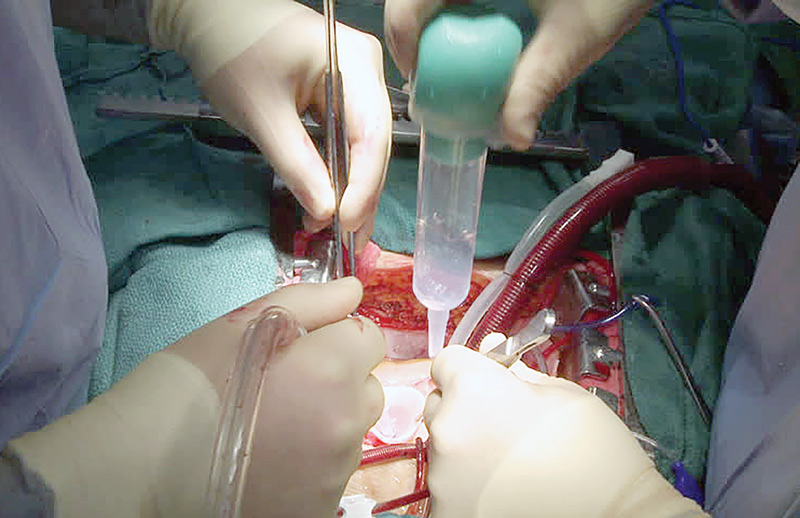
That's what Sanford Medical Center Fargo (N.D.) did recently. The facility used to rely on a variety of irrigation solutions, which were often compounded or mixed by a circulator right in its ORs. When the Joint Commission raised concerns about the safety of such an approach, Sanford took the following steps to do away with its irrigation compounding practices, according to Laci R. Soper, BSN, RN, the facility's operating room educator.
- Standardized the options. Sanford's first course of action was a detailed analysis of 50 surgeon preference cards. Throughout the analysis, certain solutions — such as a combination gentamicin-saline solution — were eliminated as Sanford attempted to standardize the solutions surgeons used.
"You need to first find out what your surgeons are willing to part with, and then go from there," says Ms. Soper.
With the help of the surgeons and clinical leaders, she gradually began eliminating the irrigation solutions Sanford surgeons could do without. In the end, the facility reduced its broad list of irrigation solutions to just three main options: A commercially available low-concentration 0.05% CHG jet lavage system, a saline solution and a pharmacy-produced antibiotic solution created in compliance with USP 797.
- Made education the priority. If you're planning on greatly reducing or eliminating a formerly compounding-heavy approach to medication distribution, you can't afford to cut any corners with the staff education component. When Sanford's standardized irrigation protocol went into effect, every member of the OR staff received comprehensive training on the change. "We make the details of our available irrigation options a focus of our education for new orientees," says Ms. Soper. "It's now one of the skills competencies we measure."
.svg?sfvrsn=be606e78_3)

.svg?sfvrsn=56b2f850_5)