A safe and speedy recovery is the result of a comprehensive process that begins long before incisions are made and continues well after patients exit your facility. From the moment patients first meet with one of your nurses for pre-operative education sessions until final physical therapy sessions are in the books, there are myriad opportunities to enhance their recoveries — and virtually guarantee they spread the word about the peerless care they received from your facility.
- Home
- Article
Recoveries Patients Rave About
By: Kern Singh
Published: 9/3/2020
Improved pre-op education, multimodal analgesia and virtual physical therapy decrease post-op pain and recovery times.
Ahead of the pain
Ultimately, positive recoveries depend on controlling patients' post-op pain in an efficient and targeted manner. Unfortunately, the pain associated with many orthopedic procedures, especially spine surgeries, is still primarily controlled with high-dosages of opioids, which is archaic and barbaric — not to mention inefficient and side-effect inducing. The good news is we're beginning to use a more targeted approach to pain control that makes low-dose opioids the last resort for post-op pain control. What's more, we're bolstering this approach with better pre-op education and more convenient and effective post-op rehab.
A multimodal analgesia (MMA) approach is the way to go. Using different-acting medications in small amounts means a smaller amount of post-operative opioids are needed, which in turn removes a cascade of negative side effects for patients. A successful MMA protocol — coupled with solid pre- and post-op patient education and rehab — is crucial for outpatient orthopedic facilities.
At least 85% of spine repairs, the specialty in which I focus, are open surgeries, which often require providers to medicate patients with large amounts of opioids afterward. Of course, opioids are also used to manage post-op pain after plenty of other common orthopedic procedures such as shoulder, hip and knee replacements and rotator cuff repairs. Patients are often given a patient-controlled analgesia pump in recovery. If they experience pain, they push the button and get an additional opioid dose. This method might relieve their discomfort, but it only treats one of the pain's pathways. Plus, the discomfort is addressed way too late in the game because the patient is already in pain and miserable. So, you're playing catchup, leading patients to consume higher doses of opioids, which cause constipation and urine retention. They're also groggy and bedridden, which can lead to post-op complications such as deep vein thrombosis (DVT), hypercoagulability or damage to the intimal vein wall.
The very premise of multimodal analgesia is that pain is not singularly mediated. Pain is actually multi-factorial and, if addressed as such, the negative effects of excessive postoperative opioids can be eliminated.
Post-op pain continues to be problematic, even with the paradigm shift from open to minimally invasive orthopedic procedures, and could prevent patients from being able to move around soon after surgery and rehabilitate faster.
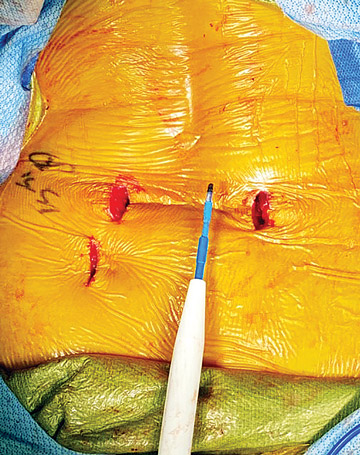
To address the pain that occurs even in a minimally invasive spine procedure — a lower back discectomy, for example — I use a generous amount of local anesthetic as a numbing medication before I make the incision, which ensures the patient's brain doesn't sense the cut being made. We use tubes to assist the insertion of the camera, which spread muscles as opposed to cutting them and reduce the amount of toxins released around the surgical site.
While anesthesia is being administered, the anesthesia provider also provides IV acetaminophen to reduce overall inflammation. Then we give very low doses of an opioid such as fentanyl to help manage intraoperative pain. After the procedure, I add more local to numb the area around the surgical site for another six to eight hours and place an ice pack on the incision to reduce swelling. We get patients up and walking as soon as possible after surgery to reduce common complications such as edemas, embolisms and DVT.
This multifaceted process all but eliminates the need for postoperative opioids. If everything is done right, most patients take only a couple of tablets for two or three days. One of the biggest premises of multimodal anesthesia is that if the patient wakes up in pain, it's too late. It means their inflammation is already high and their brain has already processed the pain.
Waking up with pain means the patient will be overly sensitive to it and afraid of it, which will lead to a need for more opioids. Waking up with little to no pain, on the other hand, is an anxiety reducing scenario.
Realistic expectations
Sending patients home nearly pain-free requires a multi-disciplinary approach. Our pre-op nurses play a critical role in patients' overall recoveries. The nurses set patients' expectations about the length of the surgery and the fact that they'll experience a small amount of post-op pain. They also explain how patients will be expected to ambulate right away after surgery, and that the amount of opioids they will be given after procedures will be minimal. The nurses then administer the first pre-op medication, generally a muscle relaxant that also acts as an anti-anxiety medication.
At our medical center, a physical therapist meets with patients an hour or two after surgery and gets them up and walking immediately if appropriate, so they don't become debilitated. After the physical therapist assesses the patient to see what their range of motion is and what their limitations are, they're given a customized home exercise program to follow, which starts with one or two physical therapy sessions done virtually via telemedicine. This is convenient for the patient because they don't have to drive to and from appointments. They can also start their physical therapy immediately, which helps to make them functional faster. For non-spinal procedures in which complications such as limb swelling takes place, there are devices to help. For total-knee replacements, for example, a wristwatch-sized device worn at the knee stimulates nerves to increase blood flow, reduce post-op edema and prevent venous thromboembolism.
Standardize to succeed
One of the top reasons our orthopedic program is so far ahead of the curve is that our anesthesia team has been phenomenal about pushing the envelope and receptive to collaborating with surgeons. Multimodal anesthesia standardizes medication types and amounts. This can insult some anesthesiologists because it removes their ability to practice "the art of medicine."
I truly believe, however, that medication practices need to be highly evidence-based, standardized and precisely protocoled. Once anesthesia teams realize multimodal protocols lead to a lack of complications, they'll see everyone's interests are mutually aligned and focused exactly where they should be — on giving the patient a quick and efficient road to recovery. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)