UNC Medical Center performed a deep dive on sterilizing and reusing these valuable protective devices. The results are encouraging but not definitive.
 CREDIT: Phillip Clapp, PhD
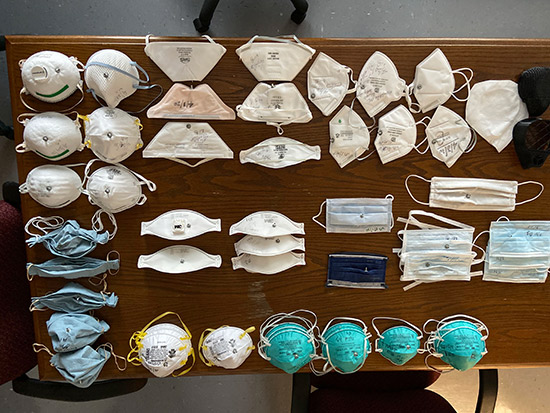
CREDIT: Phillip Clapp, PhDHANGING OUT A look at the variety of masks used in UNC School of Medicine's study of used and expired N95s.
With demand for PPE higher than ever due to the COVID-19 pandemic, many surgical facilities face the unpalatable option of reusing the N95 masks they have on hand. Just how safe is this practice of sterilizing N95 masks, and what's the best way to perform it? Researchers at University of North Carolina (UNC) Medical Center in Chapel Hill sought to find that out in a broad study that tested the effectiveness of used and expired N95 masks in keeping particles from getting inhaled. They found the masks, even expired masks in good condition, can be sterilized using vaporized hydrogen peroxide and ethylene oxide without getting compromised.
"Sterilization is more effective than disinfection for killing microbes, but we are still learning about the impact these methods have on the effectiveness of the mask," explains Emily Sickbert-Bennett, PhD, director for infection prevention at UNC Medical Center. She says more data is needed on how many times the same mask can be sterilized, a process which takes several hours. EUAs (emergency use authorizations) for some systems have tested the effectiveness of re-sterilization up to 20 times, she notes, but adds that "the impact of repeated use conditions, like long-term wear and humidity from breathing, have not been fully assessed to determine the impact of these challenges on the masks' effectiveness."
All told, after studying more than two dozen masks, the researchers found that certain N95s offer upwards of 95% effective protection. Masks as old as 11 years past their expiration date were tested. The researchers found the expiration dates largely didn't impact their efficiency, although their effectiveness likely depends on how the masks were stored.
"Masks should be stored in accordance with the manufacturer's instructions to preserve the integrity of materials," says Phillip Clapp, PhD, a UNC toxicologist who collaborated with Dr. Sickbert-Bennett on the research. "Storage environments should be clean with temperature and humidity controls."
"We tested up to 11 years past expiration and found them to still be effective masks, but there is not much data on expiration dates and it likely also depends on how the masks were stored," says Dr. Sickbert-Bennett. Also, keep in mind that not all N95 masks are created equal. "Depending on the technology, there are some material incompatibilities with sterilization," she says, recommending you check with each manufacturer about how suitable their masks are for sterilization, and how many times they can be re-sterilized, if that information is available.
The researchers emphasize that the reuse of N95 masks via sterilization should not become a permanent protocol at facilities when supply shortages cease to be an issue.
"The sterilization and reuse of masks is only being considered an acceptable practice under these emergency situations and likely will not continue," says Dr. Sickbert-Bennett. "The resources to sort, prepare, sterilize and package sterilized masks are not insignificant, and when the supply chain recovers, it will likely not be a cost-effective method."
One key factor to keep in mind when donning a re-sterilized mask is its fit, the researchers stress. A snug-fitting mask gives the most effective protection; ear-looped masks were found to be 30% less effective than masks with tie strings that go around your head. A snug mask, in good condition, properly sterilized, can offer high levels of protection. The research team laid out specific steps for UNC medical staff to take while donning an expired or used mask including to check the fit, condition and sterilization each time you put on an old mask to safeguard your personal protection.
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)