Efficient endoscope care is key to maintaining case volumes in high-volume facilities.
 CREDIT: Gateway Endoscopy Center
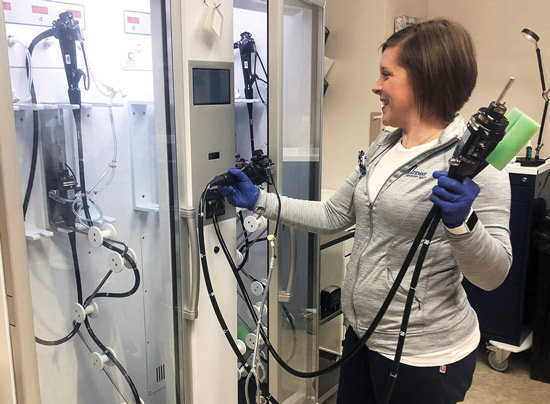
CREDIT: Gateway Endoscopy CenterEASY, BREEZY The task of ensuring channels of reprocessed endoscopes remain dry and vertical can be aided by enhanced storage cabinets with continuous airflow.
Many GI centers were hit hard by last year's pause of elective procedures and had to adjust routine practices to build case volumes back to pre-pandemic levels. Now the facilities are working at full capacity and reemphasizing expert endoscope reprocessing to keep up with the demand for colonoscopy screenings.
"We had a horrible two-month dip — an 80% to 90% reduction in screening volumes — during the shutdown, so we knew our numbers were going to be low last year," says Frank Kim, MD, a gastroenterologist at the Center for Digestive Health & Nutrition in Moon Township, Pa. "It took some convincing to get patients to return to get the screenings they needed."
The center's return to relative normalcy involved implementing updated safety protocols and clear communication with patients to ensure they had confidence in the care they received. To keep the facility running at full speed when patients started to reschedule postponed procedures, Dr. Kim's staff allotted additional time for the thorough cleaning of procedure rooms and made sure endoscopes were cared for effectively and efficiently.
Multi-society guidelines for the proper handling and reprocessing of endoscopes during the pandemic provided some guidance for facilities in a similar situation as the Center for Digestive Health & Nutrition. The steps outlined in the guidance were largely the same as recommendations in place during non-pandemic times — immediate bedside cleaning, transport in a closed container, meticulous manual cleaning and vertical storage to ensure channels remain dry — but the societies suggested limiting the number of reprocessing techs who reprocessed scopes, and making sure the techs who handled the reprocessing were experienced and had documented competencies.
"Transmission of viral infections during endoscopy is exceedingly rare and when it does occur, it is the result of noncompliance or deviation from the required steps of reprocessing," note the guidelines. So, as the pandemic showed and routine times confirm, turning around endoscopes quickly and properly is essential to providing safe and speedy patient care.
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)