This important process can help save your facility billions of dollars.
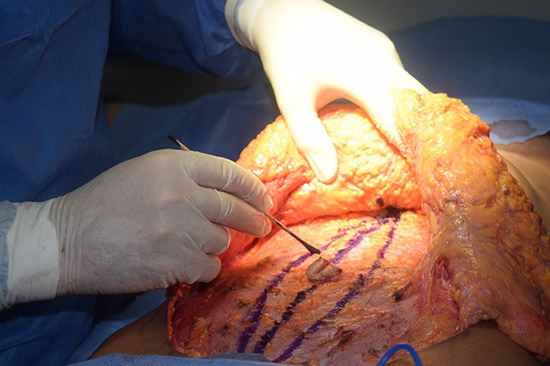
 HEAVY LOAD Pressure injuries can turn up in various locations on the body depending on surgical positioning, such as this forehead injury suffered by a patient who was in the prone position.
HEAVY LOAD Pressure injuries can turn up in various locations on the body depending on surgical positioning, such as this forehead injury suffered by a patient who was in the prone position.
According to the U.S. Joint Commission on Patient Safety, pressure-induced skin and soft tissue injuries occur in 2.5 million patients in acute-care facilities annually and result in roughly 60,000 deaths each year. Another shocking statistic? The total annual cost of pressure injuries in the U.S. was estimated to be $11 billion in 2006 and $26.8 billion in 2016, with a median treatment cost of $27,000 per injury.
When it comes to the surgical management of pressure-induced skin and soft tissue injuries, an article recently published on UpToDate says providers must identify the clinical stage of the pressure injury before proceeding. Here are those six stages:
- Stage one. Skin is intact but with non-blanchable redness for greater than one hour after relief of pressure.
- Stage two. Blister or other break in the dermis with partial thickness loss of dermis, with or without infection.
- Stage three. Full-thickness tissue loss. Subcutaneous fat may be visible; destruction extends into muscle with or without infection. Undermining and tunneling may be present.
- Stage four. Full-thickness skin loss with involvement of bone, tendon or joint, with or without infection. Often includes undermining and tunneling.
- Unstageable. Full-thickness tissue loss in which the base of the ulcer is covered by slough and/or eschar in the wound bed.
- Deep-tissue pressure injury. Purple or maroon localized area of discolored intact skin or blood-filled blister due to damage of underlying tissue from pressure and/or shear.
The reconstruction of a pressure-induced injury usually involves the creation of a flap, which can be performed during the same surgery following debridement or in a subsequent procedure depending on the amount of tissue loss, completeness of debridement, presence of infection, nutritional status and general condition of the patient, and at the surgeon's discretion. Reconstructive surgery for pressure-induced injuries is known for a high rate of complications, which can be reduced with careful perioperative care and rehabilitation within a coordinated multidisciplinary system at centers accustomed to managing these difficult wounds.
When injuries occur, employ a multidisciplinary approach during the patient's episode of care, involving everyone from plastic and reconstructive surgeons, orthopedic surgeons and anesthetists to wound care and rehabilitation specialists.
.svg?sfvrsn=be606e78_3)

.svg?sfvrsn=56b2f850_5)