The importance of properly treating incision sites ramps up after discharge.
 CREDIT:
American College of Surgeons
CREDIT:
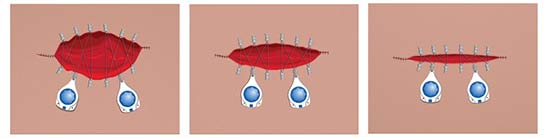
American College of Surgeons VITAL EDUCATION Surgical wounds like this can be a scary proposition for patients and their caregivers, which places the onus on providers to be proactive in educating them on how to properly care for them.
Post-op providers should focus on more than treating postoperative nausea and vomiting (PONV) and managing pain. “Patients and their caregivers are responsible for managing wounds, but there’s very little help available to guide them,” says Kathleen Heneghan, PhD, MSN, RN, PN-C, assistant director of surgical patient education at the American College of Surgeons (ACS).
With that in mind, surgical facilities must implement these pointers and protocols to ensure incisions heal properly when patients are on their own at home:
- Early information. Educating patients on how to care for surgical wounds should begin as soon as they schedule procedures, when they’re more receptive to processing the information. “They’re dealing with so much emotional stress and physical strain on the day of surgery, so it’s not a great time for learning or remembering,” says Nancy Strand, MPH, RN, manager of surgical patient education at ACS. She says it’s also important to tailor the instructions to individual patients. For instance, smokers should be told to stop smoking, which can delay wound healing.
- Show and tell. Providers should demonstrate proper ways to change dressings and clean wounds. Detailed informational packets and hands-on demonstrations performed well in advance of surgeries give patients and their caregivers the base knowledge they need to clean and prepare incision sites when the time comes.
- Clear instructions. It’s never safe to assume patients fully comprehend even the most basic care instructions, says Dr. Heneghan. Written directives about wound care — and the supplies needed to properly dress incision sites — should therefore be included in discharge packets. Providing this information in a convenient and easy-to-understand format provides patients with a handy reference during the critical stages of their recoveries.
- Contact phone numbers. It’s important for patients to reach a member of their care team if they’re concerned about the condition of their wound or the possibility of infection. Being able to call a provider to sort out if their cause for concern requires follow-up care or is part of the natural wound healing process can mean the difference between needed follow-up care and unnecessary trips to the clinic.
Giving patients the information they need to manage their wounds well in advance of their procedures will ensure they head home with the confidence to take ownership in their care and contribute to their own successful recoveries.
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)