Testing is the only way to ensure the complex devices are being cleaned properly.
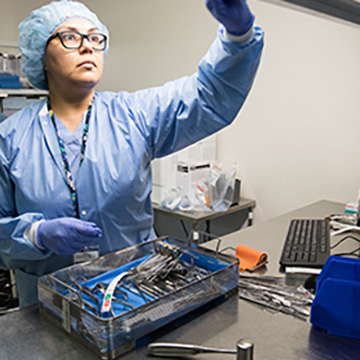
 CREDIT: Dartmouth-Hitchcock Medical Center
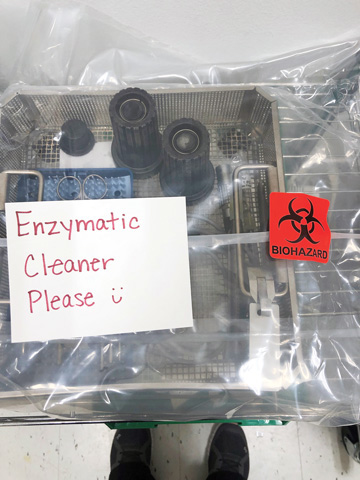
CREDIT: Dartmouth-Hitchcock Medical CenterERROR OPPORTUNITIES Failure points can take root in unexpected places under the rigorous and exacting protocols for endoscope reprocessing.
Recent FDA investigations of post-procedure infections and contamination issues involving endoscopes have reignited efforts to reprocess the devices properly.
"We've been performing risk assessments, educating teams and investing in enhanced reprocessing equipment for years to meet the many challenges involved in cleaning and high-level disinfecting these devices," says Alison Sonstelie, BS, CRCST, CIS, CHL, sterile processing lead coordinator at Sanford Health in Fargo, N.D., and president of NoCoast Consulting. "With this new round of attention, it will be helpful for administrators to refocus on basic reprocessing steps and identify potential gaps in the process."
Ms. Sonstelie lays out this roadmap:
Risk assessment. "Shadow your facility's reprocessing steps from start to finish, and solicit feedback from the frontline team members about the process," she says. "Observe bedside cleaning, manual cleaning and disinfection/sterilization practices, and compare them to your standard operating procedures and competencies." She suggests creating a multidisciplinary team to perform the risk assessment, and implementing a formal process, education plan, visual guides, checklists, points of contact and a monitoring plan.
Leak detection. "Leak testing has an important role in infection prevention because it can detect damage to the scope that may lead to fluid invasion, which increases the risk of cross-contamination," she says. "Unfortunately, it is one of the most misunderstood and frequently missed steps in endoscope reprocessing. Catching damage early will help lower the risk of cross-contamination and hopefully reduce repair costs." Automated leak testers, she adds, can help detect minor damage that may be missed during a manual leak test.
Cleaning confirmation. Adenosine triphosphate protein (ATP) testing helps to verify the effectiveness of the endoscope cleaning process. "The presence of ATP in a ‘clean' endoscope is an indicator that potentially pathogenic material is still present," she says. "To develop and implement a testing program, determine which endoscopes you'll monitor, the testing frequency, the pass-fail threshold and a standardized way to track results for process-improvement purposes."
Ms. Sonstelie says incorporating a verification program into your current practices can better identify trends and gaps in cleaning and disinfecting processes. Be sure to have a backup inventory of scopes available in the event contaminated scopes need to be removed from service, she adds.
"Endoscopes will continue to be challenging devices to reprocess," says Ms. Sonstelie. "It's imperative to first understand the standards, guidelines and best practices, and implement enhanced cleaning and disinfecting processes as needed. The ability to adapt to new recommendations and technology is the most effective way to prevent endoscope-related infections and ensure safe patient care."
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)