Cosmesis should never be an afterthought.
 CREDIT: Sherwin S.W. Ho, MD
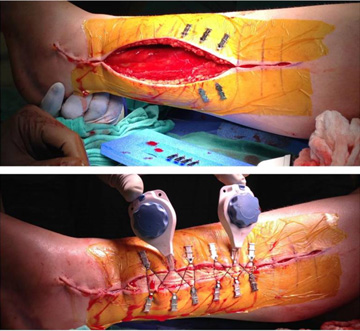
CREDIT: Sherwin S.W. Ho, MDCLOSING TIME Administered properly, emerging wound closure techniques can not only boost efficiency in the OR but, more importantly, minimize scarring for patients.
In the name of efficiency, some surgeons let their assistants close an incision so they can quickly move to the next OR and the next case. Sutures and staples get used, sometimes out of nothing more than habit. The procedure itself was a success — but it left a significant scar.
That's not best practice, according to Jeffrey S. Freed, MD, MPH, FACS, a clinical professor in the department of surgery at the Icahn School of Medicine at Mount Sinai in New York City. "I tell all my third-year medical students the same thing: The scar is often the only thing patients remember about their surgeries," he says.
Surgeons who might believe there is no reason to stop using their tried-and-true wound closure methods should be made aware of new alternatives that provide plenty of benefits, including sending their patients home with a constant visual reminder of the cutting-edge care they received. A variety of wound closure products are now on the market that result in less scarring than what commonly occurs when sutures and staples are used. These products include adhesives, adhesive and tension-distributing combinations, external tissue expanders and technology that employs tiny hooks or micro-anchors that dig into the dermis.
This new generation of wound closure products can deliver other benefits beyond minimal scarring. They can save a facility money because they take less time to use. "You can save around three or four minutes in closure time at the end of a case, which really adds up," says Sherwin S.W. Ho, MD, a professor of orthopedic surgery and rehabilitation medicine and the director of the sports medicine fellowship program at University of Chicago Medicine.
The novelty of using innovative products can also help surgical practices on the patient satisfaction front. "When you tell patients about a new device you'll use to close their incision and explain how it works, they get excited," says Dr. Ho. "These are the people who will talk to their friends and family and spread positive reviews about your facility."
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)