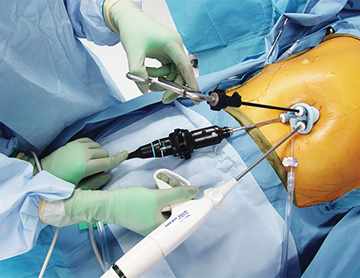
Ultrasonic shears work very well on 7mm vessels and feature adaptive-tissue technology that adjusts the amount of energy delivered to the tips based on the thickness of tissue being grasped. Curved blades on these instruments are designed to improve
visibility at the business end and the coated surfaces allow for quick and precise cutting. Ultrasonic shears are widely used to seal pulmonary vessels 7mm or smaller in procedures such as anti-reflux procedures, hiatal hernia repairs, foregut
surgeries and multiple procedures on the esophagus, stomach and small bowel.
As is the case with most electrosurgery devices, there is always a risk of lateral thermal spread injuries when these graspers are used. Extended bursts of energy delivered through prolonged activation creates high temperatures at the instrument’s
tip. If the procedure calls for immediately cutting another area of tissue, surgeons can quickly touch the tip to a piece of fat to cool it down so it’s safe for continued use.
Many physicians prefer to work with a single instrument that integrates the ability to cut tissue with ultrasonic technology and seal blood vessels with ultrasonic energy or high-frequency bipolar electrical current. These devices save time and
increase efficiency because surgeons don’t have to use harmonic scissors to make cuts and then switch to a sealing device to stop vessels from bleeding. The tips in these devices are designed for fine dissection, so they can be used
for multiple roles in a procedure such as repairs of gastric vessels during hiatal or stomach hernia procedures.
Hybrid devices are powered by a single generator, and some offer the ability to use ultrasonic and bipolar energy simultaneously for quick and precise sealing and cutting. Some devices also feature intelligent tissue monitoring technology, which
includes an auto-stop feature that cuts off the energy after satisfactory transection occurs to prevent patient injury.
Radiofrequency energy devices are indispensable tools for procedures in which vessels smaller than 1mm need resealing. They use heat-inducing technology that stops bleeding by shrinking collagen in blood vessels. The device I use combines radiofrequency
energy and saline to provide hemostatic healing of soft tissue and bone. By operating at 100°C, about 200 degrees less than many other electrosurgery devices, it does the job while reducing the amount of surgical smoke emitted into the
air.
These devices, which effectively abate bleeding from very small blood vessels, are used for liver resections, distal pancreatectomies, partial nephrectomies and colon procedures. Some monopolar sealers on the market are useful in this regard as
well. Controlling this type of bleeding reduces hematomas, improves visualization at the operative site, can reduce the need for powder hemostatic agents and results in shorter surgeries. It can also reduce post-op pain and swelling, resulting
in faster discharges. Reducing the potential need for blood transfusions during surgery limits the risk of complications, infections and hospital transfers.
.svg?sfvrsn=be606e78_3)

.svg?sfvrsn=56b2f850_5)