Protecting valuable tools throughout the entire reprocessing cycle extends their lifespan and keeps them in top working order.
 Gretchen Steelman
Gretchen Steelman
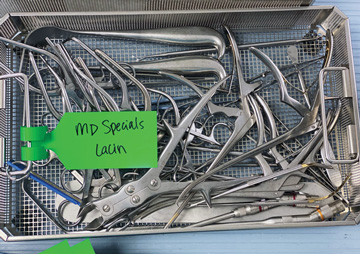
HIGH PRIORITY Green tags in instrument trays indicate to reprocessing techs that the set needs to be sterilized and returned to the OR as quickly as possible.
Surgical teams expect to work with instruments that are sterilized correctly, in pristine condition and arrive in the OR in time for cases to begin as scheduled. Making sure that happens requires streamlining workflows and rationalizing trays of often-used tools.
Placing a green placard in instrument trays that require special attention is an easy way to alert reprocessing technicians that the tools need extra care or must be fast-tracked. "The disposable placard indicates the tray needs to go to the front of the line in decontamination or that it contains specialized instrumentation that must be handled with extra care," says Gretchen Steelman, MBA, BSN, RN, CNOR, supply chain category manager at the University of North Carolina Health System in Durham. "It's a simple cue that can be used for critical sets that are limited in number or contain delicate instruments."
Additionally, Ms. Steelman's efforts to right-size the number of instruments that UNC's sterile processing department (SPD) must care for has helped to maintain the quality of tools that are in constant rotation. She and her team removed more than 10,000 instruments from 40 trays used during high-volume procedures, an effort that saved about 800 staffing hours and $10,500 in staffing costs in a year. They also repurposed 950 instruments removed from standard rotation to fill gaps of need across the health system.
She recommends tracking usage of high-volume sets that contain at least 40 instruments to determine which tools are used most often and which are used less frequently and therefore could be removed from the regular rotation. Surgeons should also be consulted to identify tools that can be removed, says Ms. Steelman. When updated, streamlined trays are created, the changes should be communicated to physician champions, sterile processing representatives, clinical managers and liaisons between the ORs and SPD to achieve buy-in and ensure the updated sets are used consistently, she adds.
"Given the increasing cost constraints in health care, we found that instrument tray reduction was an untapped resource for cost savings," says Ms. Steelman. "We continue to look into instrument rationalization for our other service lines and plan to consolidate some trays that could create even more cost improvements."
Ms. Steelman also points to the benefits of using rigid sterilization containers, which offer increased protection and are a better option for keeping tools organized than standard blue wrap. Some sterilization containers come with optional baskets and inner liners with slots designed to house individual specialized instruments.
.svg?sfvrsn=be606e78_3)



.svg?sfvrsn=56b2f850_5)