Patients are seeking more procedures in breast and abdominoplasty as they look to improve their overall well-being and health.
 Tripp Holton, MD
Tripp Holton, MD
Tripp Holton, MD
The demand for plastic surgery has increased since the beginning of the pandemic for a variety of reasons including a renewed focus on health, improving mental and physical well-being and the opportunity to
recover at home. According to a new national survey conducted by the American Society of Plastic Surgeons (ASPS), cosmetic procedures have increased with young women responsible for the steady uptick in procedures.
Three-quarters of the society's member surgeons report that their practice volumes are increasing, with 30% reporting their business has at least doubled.
Outpatient Surgery Magazine spoke to Tripp Holton, MD, a plastic surgeon in Annapolis, Maryland who is affiliated with Luminis Health Anne Arundel Medical Center to talk about the trends in plastic surgery today.
Q: Your specialties are breast reconstruction including reconstructive microsurgery as well as cosmetic plastic surgery of the face and body. Have you seen an increase in patient interest in these areas and what do you think is driving that demand?
For my practice there has been a noticeable increase in demand for aesthetic procedures since early after the beginning of the pandemic. Initially, this seemed to relate to patients' inability to travel (domestic and international) and
possibly to bonuses of money associated with PPP loans, etc. Interestingly, in particular, there was an uptick in injectables and procedures for areas of the face not covered by masks such as the forehead and upper and lower eyelids
as these areas remained visible. However, the trend seems to have continued beyond mask mandates, travel restrictions, strictly enforced social distancing and shelter in place recommendations. While our Millennial and Generation Z
populations are lauded for valuing experiences over "things," they seem to also value looking great when they do experience things and certainly when they share their experiences visually on social media.
Q: What are the challenges of performing successful breast reduction surgery?
Breast reduction surgery is a commonly performed procedure nationally and certainly my practice echoes that trend. I refer to these procedures as "cosmedical" because they are medically necessary to address back, neck and shoulder pain
while simultaneously inherently cosmetic because patients have an understandable interest in maintaining or achieving a symmetric, attractive and harmonious appearance after the surgery.
Symmetry after breast reduction does not only mean breast volume but also the position and diameter of the nipple and areola and the shape and drape of the breasts.
Achieving symmetry, often when the breast started with significant asymmetry, can be a challenge. Additionally, breast reduction surgery is invasive and requires a tremendous amount of dissection, suturing and wound healing and, accordingly,
the greatest challenge to the surgeon is likely guiding the patient through the often lengthy and intensive process of healing.
Q: For abdominoplasty can you describe the challenges here? Are these higher risk surgeries?
Abdominoplasty or "tummy tuck" surgery which is often combined with liposuction in the region (flanks, back and/or upper abdomen) is a high yield procedure associated with tremendous patient satisfaction, but it can be complicated by issues
such as bleeding, asymmetry, widened, raised or discolored scars, wound development and most concerning but fortunately rare deep vein thromboses (blood clots). Excellent aesthetic results after abdominoplasty hinge on competing factors:
to remove as much extra skin and fat from the region as possible the surgeon must then close the incision under moderate to large amounts of tension. Too little tension typically means that not enough tissue was removed, and the result
is accordingly disappointing whereas the removal of a bit too much tissue can result in more complications such as wound development and issues with the appearance of the scar.
Q: What do you do to keep the patient safe from infection and complications?
The patient is paying the surgeon for two often competing goals: they want the best looking result and they expect to be kept out of harm's way. To accomplish these competing priorities, I rely heavily on experience, judgement and technology.
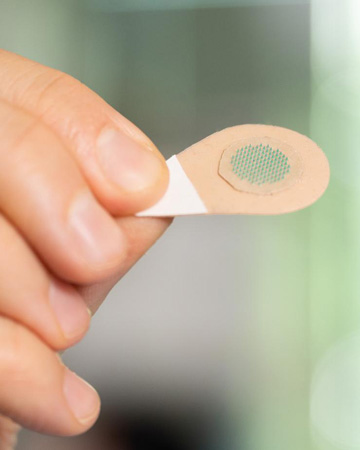
In particular, I ask a lot of the dressings that I use in abdominoplasty and breast reduction surgeries. Specifically, I typically use closed incision negative pressure dressings because they do several critical things for me and by
proxy my patient. These advanced dressings actively manage the incisions and the surrounding soft tissues: they off load tension across the incisions, reduce swelling within and below the skin, increase blood supply to the tissue and
protect the incision from contamination by creating and maintaining a sealed and sterile environment after the surgery.
Q: For wound care, what do you see as the best practices?
While wound care is a critically important process, I strive for and focus on active incision management because the Holy Grail of cosmetic surgery is to manage incisions to prevent the development of wounds. I have personally enacted
a zero-tolerance policy for wound development after cosmetic procedures. To help achieve this austere but important goal I mandate that all tummy tuck and breast lift patients are managed with an advanced incisional management dressing
such as a 3M™ Prevena™ Dressing along the waistline closure after abdominoplasty and a 3M™ Prevena Restor™
BellaForm™ Dressing to cover the breast after a lift especially when an implant is placed at the same time.
Q: Are you seeing more patients seeking combination procedures and what does that mean for your preparation?
Combination procedures are common. Typically, when a patient has cosmetic issues in one location they have those same issues in another region. I will often perform a breast lift and a tummy tuck or a tummy tuck and a thigh lift with or
without liposuction, but I never combine more than two areas per procedure.
A little more than a decade ago surgeons were still commonly performing combined procedures informally known as total body lift, but we eventually recognized that this approach exposed patients to unnecessary risk in the form of required
transfusions, infection, increased likelihood of wound development and challenges with controlling pain.
While many of my patients could benefit from procedures in more than one location, I generally limit them and myself to two regions at time. While this means more than one surgery and possibly incrementally more expense it rewards the
patient with better results and fewer complications. It also allows the surgeon to revise the initial procedures while performing subsequent operations. In these cases, I am careful to optimize their care with adjunctive therapies
such as regional pain blocks and advanced dressings.
Q: What do you see as the most important new trends in plastic surgery?
I have always believed that advancements in technology allow advancements in techniques. Recent trends in breast reconstruction for cancer provide an excellent example of how intelligent use of technology has informed our choice of surgeries.
When I trained and when I was first in practice all of my implant-based breast reconstructions after mastectomy started with placement of a breast tissue expander beneath the patient's pectoralis major muscle. This was then followed
by a series of visits for expansion and culminated in a second operation to replace the temporary device (tissue expander) and place a permanent implant into that pocket.
In 2016, I began to build all breast above the muscle since we finally had technologies that made that possible such as blood supply mapping, excellent tissue for implant support, higher quality breast prostheses and, importantly, dressings
that protect the breast while improving the nascent blood supply. Shortly after switching to this new approach (pre-pectoral reconstruction) I learned that almost all of my patients could be accelerated to placement of an implant immediately
rather than requiring an expander and the associated visits for expansion and final operation to exchange the expander for an implant. Now, technology had allowed the breast to be made in front of the muscle (far less pain) and with
the immediate placement of the implant. With patients in far less pain we were suddenly able to safely and compassionately send patients home on that same day.
I see technology helping my cosmetic patients in much the same way. I, and now they, expect to be back to normal activity very soon after surgery.
Q: What advice would you give fellow surgeons and OR teams in the outpatient environment to create a successful practice?
As hospital systems nationwide move rapidly towards diverting less complex cases from the hospital operating rooms into high quality but lower cost ambulatory surgery centers, the intelligent practice will prepare to use these advanced
technologies and supplies in that outpatient setting. When insurance-based care is transferred to the ambulatory care environment advanced therapies in the form of regional pain care and advanced dressings become even more valuable
– adept practices will adapt by adopting intelligent approaches and technologies.
NOTE: For more information please go to 3M.com/PrevenaCentral
Note: Dr. Holton is a consultant and speaker for 3M due to the value that he places on the 3M products designed for management of incisions, tissue and wounds.
 TRANSPARENT TALK Patients and surgeons considering breast implantation should be aware that squamous cell carcinoma and various lymphomas could form around scar tissue.
TRANSPARENT TALK Patients and surgeons considering breast implantation should be aware that squamous cell carcinoma and various lymphomas could form around scar tissue..svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)