- Home
- Article
Bridge Technology and Training to Improve Instrument Trays
By: Carina Stanton | OSM Contributor
Published: 4/2/2025
AI-assisted technologies can curb tray assembly headaches and infection risks.
Missing instruments. Wrong instruments. Contaminated instruments. Each creates a losing proposition for surgery, from costly delays to frustrated OR staff and surgeons to patient infection risks.
“In some sterile processing departments, chronic understaffing and the staff not always being properly trained due to high turnover rates or short tenure are often found to be major contributors to instrument tray management issues,” says Peter Graves, BSN, RN, CNOR, infection prevention consultant and CEO of Clinical Solution in Anna, Texas.
Mr. Graves observes tray assembly quality as a significant operational challenge for outpatient surgery leaders. It also poses a major infection risk that he and his infection prevention colleagues have educated teams on widely, including the issue of increased OR traffic in and out of the room to retrieve missing instruments.
Research investigating the causes of surgical site infections has found air to be a major exogenous source for infection, as airborne particles in the OR contaminated with live bacteria can enter the sterile surgical field during a procedure. This is a particular risk when implants are placed during total joint replacements.
“Whenever the OR doors are opened during a surgical procedure, no matter the reason, it changes the positive air pressure and can create turbulence within the OR suite that can place the patient at unnecessary risk for a surgical site infection,” notes Mr. Graves.
Despite obvious challenges, Mr. Graves is optimistic about what can be done. He’s not alone. Perioperative leaders are finding creative solutions centered equally in increasing knowledge of evidence-based practices to curb infection rates and leveraging technology advances, including AI and automation.
Explore automated tray management solutions
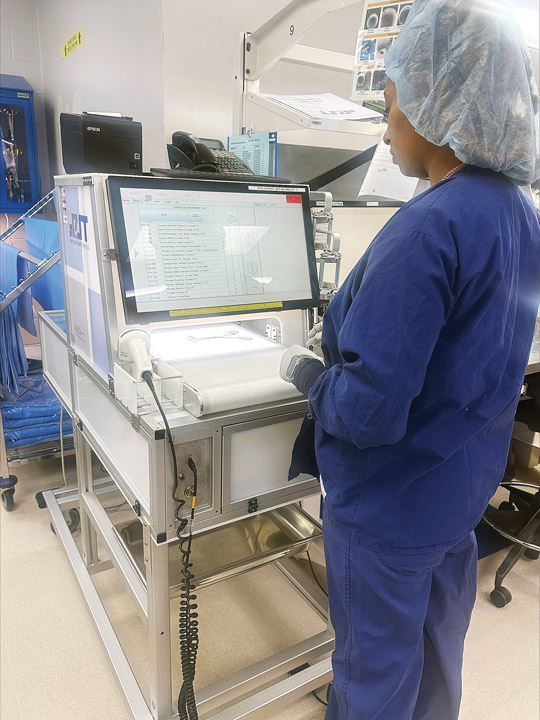
AI-driven machine vision technology is helping sterile processing departments overcome the operational challenges of instrument tray management. For example, AI-driven technologies currently on the market can help a sterile processing technician, even one new in their role, assemble 150-instrument complex surgical trays quickly and accurately, a task that was previously reserved for more experienced technicians.

Sterile processing team members need the right tools and training to optimize instrument management. Here’s how leaders can structure their approach to meet these needs, according to Densley Coke, MBA, BSHM, CST, CRCST, CHL, CER:
• Invest in technology. Tools with AI automation can significantly improve accuracy and efficiency in instrument tray management.
• Foster communication. Establish clear lines of communication between the OR and SPD to proactively address issues and maintain trust.
• Standardize processes. Create consistent tray setups and documentation to reduce variability and errors.
• Enhance collaboration. Involve OR staff in discussions about new technologies and workflows to ensure alignment and mutual understanding.
• Prioritize safety. Pair automation with manual quality checks to achieve the highest standards of accuracy and safety.
—Carina Stanton
AI can also serve as a second set of eyes to catch missing or incorrect instruments found on surgeon preference cards. Some technologies automate peel packs and target sterility with all-in-one rigid sterilization containers that can be transported directly to the OR.
Cleaning verification with AI provides another game changer in sterile processing to help assess performance. Last year, the Association for the Advancement of Medical Instrumentation (AAMI) described this technology as “one of the most promising (and potentially disruptive) technologies of the modern age.”
Beyond sterile processing, Mr. Graves notes that implementing advanced technologies such as AI-driven machine vision for tray assembly can ensure consistent and accurate preparation of instrument trays. This can help in the OR by addressing the root causes of incomplete instrument trays, thus reducing the need for staff to leave the operating room. Some automated systems he’s learned about also can generate a significant amount of data, which he sees as valuable to help drive change and further quality improvements.
One facility finding improved efficiency and safety benefits with automated instrument tray management is Northside Hospital Forsyth in Cumming, Ga., says Central Sterile Processing Manager Densley Coke, MBA, BSHM, CST, CRCST, CHL, CER. During his 32 years working in sterile processing, he’s seen technology evolve, but nothing as transformative as what’s happening today with AI automation.
In 2024, his team implemented instrument tray automation to streamline tray assembly, peel pack preparation and storage processes. He led the implementation successfully with these five strategies:
1. Communication. He and his team clearly and frequently communicated about the implementation process. This included timelines that helped build trust with staff and minimize resistance.
2. Team education. Training on the technology was rolled out in phases. It combined vendor-led demonstrations with hands-on practice and simulation exercises. “We empowered team leads to become system champions, offering peer support to colleagues,” says Mr. Coke.
3. Workflow adjustments. Closely examining and modifying workflows helped integrate the system’s capabilities into daily practices. Regular huddles and feedback sessions during implementation allowed for iterative improvements.
4. Assessment and customization. The team collaborated with the automation system vendor to assess workflows and customize the system for specific needs. This has ensured a seamless fit with existing processes.
5. Individual staff support. By providing one-on-one guidance with individual staff members, those who were hesitant gained understanding of how the automated system would improve efficiency and patient safety.
Encourage critical thinking

Mr. Coke believes that technology alone is not the answer. From a leadership perspective, he continues to focus on processes to ensure every new automation feature is validated against AAMI and CDC guidelines, as well as to ensure the system supports, rather than compromises, best practices. He stresses the value of confirming the technology’s work. “While our automation system enhances efficiency, manual inspections and quality checks remain integral to our processes. This dual oversight safeguards patient safety,” he says.
Mr. Coke is a strong advocate for helping his team lead their work with evidence-based practices and to use the technology to enhance and streamline what they do. “We empower our team to question outcomes and report discrepancies, reinforcing their role as knowledgeable professionals,” he says. He and his perioperative leader colleagues provide ongoing training across sterile processing and the OR on infection prevention and sterile processing principles, ensuring team members understand the science behind the technology.
This infection prevention know-how is essential, according to Mr. Graves, because inadequate cleaning, sterilization and instrument handling remains a concern given the risks they pose to patient safety.
Contamination risks when managing instruments
When instruments are not thoroughly cleaned, inspected and sterilized, microorganisms and other infectious materials can remain, posing a significant infection risk to patients and jeopardizing the healthcare institution’s safety standards. Two areas where Mr. Graves sees safety concerns during sterile processing include when understaffed or undertrained technicians incorporate errors in the sterilization process, and when instruments are mishandled during decontamination and packaging, which can introduce contaminants. “Proper protocols and rigorous training are essential to mitigate these risks and ensure patient safety,” he stresses.
Additionally, wrapped instrument sets present unique challenges. “If the wrapper becomes soiled, wet or suffers a breach, it compromises the sterility of the instruments,” explains Mr. Graves. Inspecting the wrapper before delivering the instrument to the back table is crucial. However, “holding up a wrapper for visual inspection can introduce dust and microorganisms into the operating room air, posing a potential infection risk,” he says.
Based on the evidence outlined by the Association of periOperative Registered Nurses (AORN) in its guideline recommendations for sterile processing, instrument packaging and sterile technique — as well as in expert guidance from CDC, the International Society of Infectious Diseases and other evidence-based recommendations — Mr. Graves suggests following these best practices for handling and inspecting wrapped instrument sets:
• Safe storage. Store wrapped instruments in clean, dry and dust-free areas to maintaining sterility. Prior to transport, staff must carefully inspect the wrapper for any signs of damage, moisture or contamination. They also must handle wrapped sets with clean, dry hands to avoid introducing contaminants.
• Contaminant-free transport. Instruments can be exposed to pathogens if not transported in sealed, sterile containers. Also, contact with non-sterile surfaces or environments during transport can lead to contamination.
• Proper handling in the OR. Handle instruments with sterile gloves and do not place them on non-sterile surfaces to prevent introducing contaminants. Minimize opening OR doors during procedures, which can disrupt positive air pressure and allow airborne pathogens to enter. Follow proper aseptic techniques to prevent the patient’s own flora from contaminating the surgical site.
“Addressing these risks involves strict adherence to sterilization protocols, proper training for OR and SPD staff, secure transport methods and maintaining a sterile environment in the OR,” says Mr. Graves. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)