- Home
- Article
Cataract Reimbursements and Beyond
By: Jared Bilski | Editor-in-Chief
Published: 7/3/2025
Lasers, LASIK and upgrades are key to survival in the ophthalmic space.
Cataract cases are among the most common, efficient and safe procedures in outpatient surgery. Between 3.5 and 4 million patients have their cataracts successfully removed each year, and complications are rare. Ophthalmic facilities and their specialized teams have worked tirelessly to make sure these high-volume cases are seen by prospective and current patients as hassle-free, life-changing procedures.
The reimbursement these hard-working providers receive for their efforts, unfortunately, leaves much to be desired.
Bilateral cataract surgery is just one example of the gap between the safe, efficient care ophthalmic centers provide to patients and the disconnect from payors in how they are reimbursed. “Insurance reimbursement can be challenging, which is one of the reasons why more centers don’t do bilateral cataracts,” says Michael J. Shumski, MD, MSE, a cataract and refractive surgeon with Magruder Laser Vision in Orlando, Fla. “Surgeons recognize the benefits and safety of same-day bilateral cataract surgery. However, insurance does not reimburse as much for the second eye, and centers face a reduction on the second eye.”
When you factor in the way reimbursements have fallen over the past five or six years, an inflationary economy and steadily rising costs, Dr. Shumski, who also serves as the medical director for “Best Cataract Surgeons”, understands why many centers don’t perform bilateral cataract cases. After all, it’s hard to justify doing both cataracts on the same day and taking a reimbursement hit when they can just do one at a time and get paid more it. This is all the more frustrating when you consider who benefits most. “For suitable patients, same-day bilateral cataract surgery is very advantageous,” he says.
“These are the patients who are expected to have very good, very quick recoveries and excellent post-op Day 1 vision. We won’t do both eyes if the patient’s vision will be extremely blurry.”
An unsustainable model
Standard cataract cases can be a losing proposition for many ophthalmic facilities. To properly understand the “why” and “how” of the current landscape, you need to zoom out and look at what’s been happening for ophthalmic practices and physician-owned ASCs year after year.
“The Medicare cuts have been draconian. Between 2020 and 2025, practices have seen a 19.8% reduction in physician fees while inflation and costs have continued to rise,” says James Loden, MD, a fellow-trained LASIK specialist who is the founder and president of Loden Vision Centers, an ophthalmology practice with five locations in the greater Nashville area. “Payroll, rent, electric and gas have gone up, insurance costs have shot up exponentially and the cost of goods are up 10 to 20 percent.”
Dr. Loden’s practice is a well-oiled machine when it comes to cataracts. It can perform these cases with a total turnover in the ASC of just one hour and 30 minutes from arrival to discharge — and sometimes in as little as one hour when “staff can really make it roll.” Despite fine-tuning and perfecting his processes, Dr. Loden, who also serves as a clinical assistant professor in the Department of Ophthalmology at the University of Tennessee College of Medicine, is pragmatic about what facilities are up against. “It’s really difficult to run a private practice without upgrades and premium IOLs,” he says. “Financially standard cataracts aren’t worth doing without upgrades unless you are performing them in your own ASC.”
“There seems to be more micromanagement of late from insurance companies in the form of prior authorizations and reimbursement cuts.”
—Michael J. Shumski, MD, MSE
Reimbursement challenges extend well beyond simple cataract cases for providers. Dr. Loden has had to stop performing full thickness corneal transplants and certain glaucoma cases because he can’t break even on them.
On a macro level, Dr. Loden sees private practice ophthalmology providers facing an inflection point. Competing with larger health systems is becoming a zero-sum game. They have the ability to pay more because of the encounter fees they receive, a fee that private practices don’t get. Plus, physicians are finding they can make more as hospital employees than they could on their own. But there will always be the case for physician autonomy, something that providers often surrender for the supposed security and stability of working for someone else.
“I’ve seen many friends who seem to have lost a lot of autonomy after taking on a new boss in the form of a health system or private equity group,” says Dr. Shumski. “In another sense, the insurance companies can be a boss because they dictate what’s covered and what’s not covered, and there seems to be more micromanagement of late from insurance companies in the form of prior authorizations and reimbursement cuts.”
Maintaining the mission
Despite daunting challenges, private practice physicians like Dr. Shumski and Dr. Loden have found success by focusing their efforts and becoming top providers in their respective areas. For Dr. Shumski, it’s a straightforward philosophy. “Our mission is to offer modern cataract surgery of the highest quality possible,” he says. Bilateral cataracts for every suitable patient makes sense for that mission. “We’ve decided it’s something for us to offer,” he says. “We have our own center, so we get to make this decision on our own, and we feel that the benefits to the patients outweigh reduced reimbursement to our practice.”
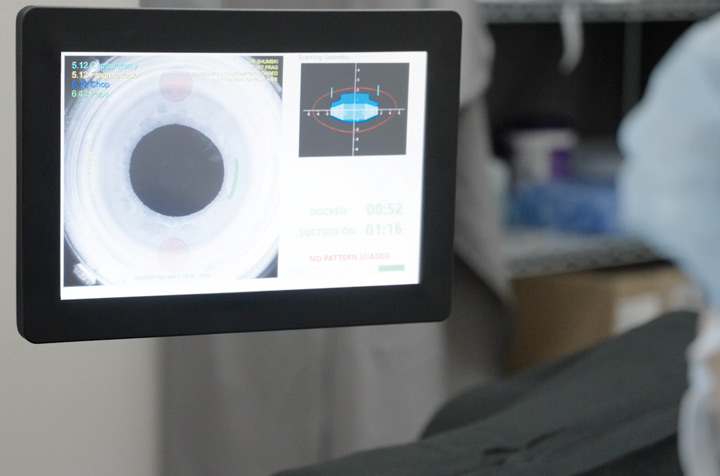
Several factors have played key roles in Dr. Shumski’s success. First, technological advances have bolstered patient safety. “The lasers have made modern cataract surgery so safe,” he says, touting equipment that has been a game changer for his practice.
There’s also the anesthesia component. “I would say I do 95% of my patients with oral sedation,” he says. “We offer IV sedation to patients when we think it’s more appropriate, but for most, oral is a better sedative.” Finally, Dr. Shumski is a strong proponent of strategically using the physical space in which procedures are performed. In other words, you don’t need be at an ASC to run a successful ophthalmology practice. “Office-based suites are another reason that we can do what we do,” he says. “The cost of opening and operating an office-based surgical suite is considerably less than an ambulatory surgery center. Savings on all those operational costs allow us to be more economically efficient.”
As someone who started his own practice in 1999 and hasn’t looked back , Dr. Loden urges younger physicians and facility leaders to expand their services as much as possible. “General ophthalmology practices must be in the refractive service game to succeed. They need to do non-covered, cash-pay cases,” he says. “Facilities have to find ways to diversify their income streams.”
Dr. Loden says lasers, premium service offerings, the ability to upgrade cases and perform procedures such as light treatments for age-related macular degeneration are all components of a successful practice in today’s reimbursement landscape.
Above all, Dr. Shumski says it’s important to remember the ultimate driver: providing quality patient care. “We all got into medicine to do what’s right and what’s best for every patient,” he says. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)