- Home
- Article
Drug Advances Improve Eye Surgery Outcomes
By: Carina Stanton | Contributing Editor
Published: 2/14/2024
From topical eye anesthetics to improved pre-op sedation to pupil dilation, medication advances are streamlining cases.
A comfortable patient who is ready for eye surgery is essential for the provider to achieve an optimal outcome. Advances in ophthalmic drugs are helping anesthesia providers and surgeons create this environment for their patients better than ever before, according to two surgical leaders in the field.
The mix matters
Robert J. Weinstock, MD, a surgeon who is recognized for eye surgery advances, leads The Eye Institute of West Florida, a high-volume multicenter outpatient practice near Tampa. His patients undergo a wide range of eye surgeries, including procedures for cataracts, glaucoma, LASIK and vison correction, as well as aesthetic procedures.
Jay Horowitz, CRNA, APRN, is chief anesthetist at Newsom Eye, also headquartered in the Tampa area, where 40 cases a day in one center can be the norm. Cataract surgeries are common procedures across the practice, and are sometimes combined with other procedures, such as those for glaucoma treatment.
Both agree that the right medication mix — largely focused on topical anesthesia, effective dilation and optimized sedation timing — is essential for a high-volume practice. Often included in the mix is a combination of cutting-edge and well-established drugs.
Preoperative drugs
Once admitted, patients should be made comfortable, numb and dilated in an efficient manner, stresses Mr. Horowitz. Dr. Weinstock says while dilation has traditionally been the most time-consuming step, medication advances are driving dilation times down. Here’s what both providers use to prepare patients for ophthalmic surgery:
• Pledget cellulose sponge. Indicated for most patients, this very small sponge (1 cm x ¼ cm) is soaked with an antibiotic, a local anesthetic and a steroid. Placed in the trough between the lower inner eyelid and eyeball — a.k.a., the lower conjunctival fornix — this drug delivery method numbs the patient’s eye without requiring a nurse to administer multiple drops in pre-op.
• Epi-Shugarcaine. This compounded drug mix, which combines bisulfite-free epinephrine and preservative-free lidocaine, is a go-to for combined dilation and numbing. It is typically administered by the surgeon into the anterior chamber between the cornea and iris at the onset of surgery. The epinephrine can help control bleeding in combined cataract/glaucoma procedures that require a stent.
The ultimate goal is getting our patients comfortable and dilated to streamline surgery and prevent delays.
Robert J. Weinstock, MD
• Oral sedation with MKO melt versus IV sedation. A lozenge that dissolves under the tongue can provide sedation. Drugs such as midazolam, ketamine and ondansetron (an anti-nausea medication) help the patient relax before surgery and recover afterward without the need to start an IV.
Mr. Horowitz cautions that these oral medications are less predictable in terms of efficacy and onset. Instead, he uses IV midazolam as a sedative to “get the best vein-to-brain responses” that will help the patient experience eye surgery comfortably. Mr. Horowitz adds that smokers and other patients who are more likely to cough must remain still during surgery and may be provided an orally administered Tessalon Perles preoperatively or 50 to 100mg IV of lidocaine intraoperatively.
Intraoperative drugs
Advances in the drugs used during eye surgery are helping to reduce or prevent complications such as inflammation. Specifically, Dr. Weinstock notes these newer, FDA approved options:
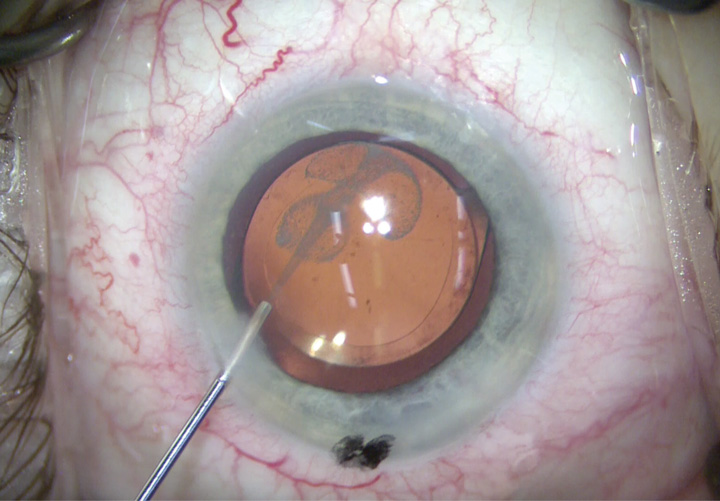
• OMIDRIA, a combination of phenylephrine and ketorolac intraocular solution, is a non-steroidal anti-inflammatory drug mix surgeons can use to irrigate the eye during surgery. It blocks receptors responsible for intraoperative and postoperative inflammation. Combined with epinephrine irrigation during surgery, it can help maintain dilation, especially if a patient is taking medication like tamsulosin to prevent dilation for other conditions such as urinary incontinence.
• IHEEZO is a chloroprocaine hydrochloride ophthalmic gel that provides ocular surface anesthesia. Although Dr. Weinstock prefers standard drops for anesthetic and dilation, he says some surgeons compound a mix of dilation and anesthetic meds. “The ultimate goal is getting our patients comfortable and dilated to streamline surgery and prevent delays,” he says.
The right approach optimizes recovery
Medication types, mixes and administration impact patient recovery and healing. In the immediate postoperative period, the benefits of short-acting sedation, local anesthesia and experienced surgeons who can complete common procedures such as those for cataracts in three to four minutes allow for expedient discharge, says Mr. Horowitz. Most of his patients are up and walking with assistance within 10 minutes after surgery to visit an in-house optometrist for a post-op check.
Dr. Weinstock says that once surgical patients go home, providers are trending toward prescribing compounded medications that combine a postoperative antibiotic, steroid and non-steroidal anti-inflammatory. The idea is to simplify recovery and improve patient compliance. This can be especially helpful when a patient’s insurance requires generics with varied dosages of individual medications, he notes. By instead prescribing one compounded medication, providers can better ensure patients are receiving the correct postoperative menu of medications to expedite healing. It can also help streamline the discharge process.
Surgery centers, says Dr. Weinstock, should engage with and use a trusted compounding pharmacy with strict protocols in order to reduce the risk of toxic anterior segment syndrome, an acute postoperative inflammatory reaction that can delay recovery and, in certain cases, pose a severe risk to the patient’s vision.
On the horizon
In terms of additional drug advances in the pipeline, Dr. Weinstock is eyeing a few developments and trials. Of most interest:
• Sustained-release ocular drug delivery systems. These small implantable devices come embedded with medications and are produced in several different forms by various manufacturers. They hook over an ocular implant and then provide time-released administration of their medications. Increasingly installed during glaucoma procedures, these devices can also come embedded with anti-inflammatory medications.
• Compounded intraoperative drugs for cataract surgery. Different combinations of compounded drugs such as trimoxifloxicin, dexamethasone or ketorolac are designed to be delivered at the end of cataract surgery. They would replace the typical postoperative approach of administering these medications separately, so they have the potential to streamline post-op care and more immediately optimize recovery.
Beyond medications
While drug advances continue to optimize eye surgery on many fronts, Mr. Horowitz stresses the equally important element of team coordination to achieve optimal outcomes. Every member of his perioperative team knows their specific responsibility to the patient. “We have found simple yet effective practices such as using a color-coded sheet attached to the stretcher that signals specific cases and related needs, such as glaucoma, cataract or astigmatism procedures,” he adds. “Everyone knows what they are looking for and are cross-trained to execute their assigned roles in concert, much like every instrument in an orchestra.”
At the end of the day, says Mr. Horowitz, the ultimate goal is a superior patient outcome that improves their quality of life. “Advances in medications, as well as lenses and other technological developments, are helping us achieve this for our patients,” he says. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)