Using a smoke evacuation system benefits healthcare workers who are exposed to chronic second-hand smoke and health risks every day.
 Steris®
Steris®STERIS
™ STERIS Smoke Evacuation unit.
™
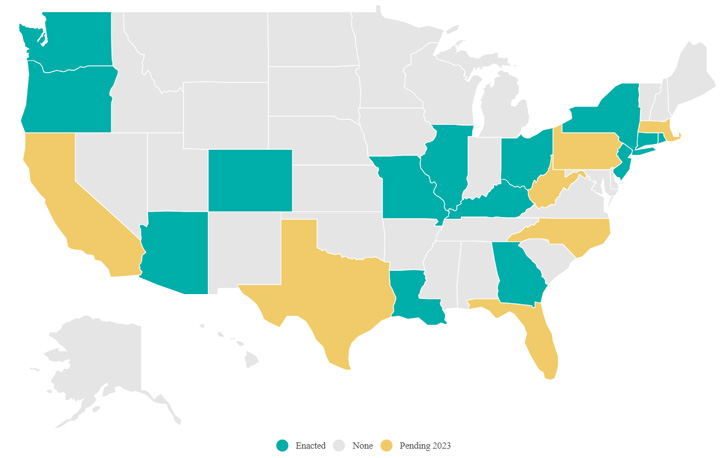
According to the Association of periOperative Registered Nurses (AORN), the average daily impact of surgical smoke on an OR team is equivalent to inhaling the smoke of 27 to 30 unfiltered cigarettes. AORN has led the fight in preventing the risk of surgical smoke for healthcare professionals who provide safe surgical care for their patients every day. That effort includes guidelines for smoke evacuation, education and lobbying efforts across the country. The momentum is growing as 11 states have passed legislation to protect the workers that put themselves at risk every day in the OR (see Article | Outpatient Surgery Magazine (aorn.org).
Until just a few years ago, policies for smoke evacuation in the operating room have been left up to the discretion of the individual healthcare facility and its leadership. That appears to be changing with states either enacting or proposing surgical smoke regulations requiring operating room (OR) environments to be smoke-free for the benefit of both patient and staff safety.
What is surgical smoke? Surgical smoke, or surgical plume, is the vaporization of substances (e.g., tissue, fluid, and blood) into a gaseous form. It is dangerous because it can contain toxic compounds, bioaerosols and live or dead cellular material, including viruses and bacteria. Smoke is comprised of 95% water and 5% other particulates, gases and microorganisms. Although the water vapor itself is not harmful, it acts as a carrier for the hazardous chemicals in surgical smoke.
Surgical smoke is produced by using lasers and electrosurgical units (ESUs) and is a byproduct of human tissue contact with mechanical, heat-producing medical devices, such as electro-surgery knives, commonly used for dissection and hemostasis. Surgical smoke exposes OR staff to biological contaminants, including aerosolized blood. Constant exposure can result in serious health issues for the doctor, support staff and patient.1 Studies have identified the presence of bacteria, HPV and viable malignant cells in surgical smoke, reflecting the importance of smoke evacuation and respiratory protection.
Today, facilities can use highly effective devices that are easily implemented in their ORs and systems to create surgical smoke evacuation – capturing the plume at the incision site and helping to prevent it from remaining in the patient or being inhaled by staff members.
How can this be done? Surgical smoke evacuation is the act of removing the plume caused by lasers and ESUs during a procedure. A common misconception is that implementing smoke evacuation will involve construction to redesign the room or even an HVAC overhaul, but this is not the case. A high-flow vacuum generates suction to collect the smoke while a filter removes the harmful particles and traps fluids within the smoke evacuation unit.
These devices can be portable on a cart or even standalone when placed on a surgical boom. While other methods of respiratory protection, such as a HEPA respirator (N95) mask and exhaust ventilation in the OR, are often in place, a more effective way of controlling surgical smoke is through the use of a smoke evacuator. The National Institute for Occupational Safety and Health (NIOSH) recommended that smoke evacuation be used in addition to general room ventilation to control smoke emission better – preventing it from reaching the breathing zone of healthcare workers and patients – and reducing the workers’ continuous exposure.
Smoke evacuation systems collect and filter the plume from electrosurgical or laser procedures at the surgical site. A typical smoke evacuation system includes a suction pump motor, sensors for activating the system, filters for trapping and purifying surgical plumes, smoke evacuation tubing, and an ESU smoke evacuation pencil. A highly effective system includes smoke evacuation tubing that slips over the electrosurgery pencil in the surgeon’s hand, allowing the tubing to be positioned to remove plumes directly at the incision site before they can escape.
Filtering capability and suction power play a significant factor in the effectiveness of the system. The types of smoke evacuators that tend to be preferred by OR teams possess a high-flow vacuum but emit a low sound level while in operation to minimize noise distractions during surgery and allow OR teams to communicate without interference.
The STERIS Smoke evacuation system is one of these such technologies available today. The STERIS smoke evacuator has improved technology and delivers a highly effective method of collecting and filtering smoke produced during either open or laparoscopic procedures. A high-speed, brushless motor helps create suction pressure up to five times greater than other evacuators, quietly pulling smoke particles expelled from the surgical site and capturing them before they can escape. It works with all surgical cutting devices found in operating rooms, and the patented electrocautery pencil with an integrated surgical smoke evacuation mechanism captures surgical plume right at the source to improve patient and staff safety.
The use of a smoke evacuation system is not only a benefit to the health and safety of everyone in the OR, but also is becoming a legal requirement in a growing number of states. Advances in technology and reducing risk are making it easier to overcome the challenge of implementing this type of device and provide a safer environment for everyone.
References:
1. Katoch, S., & Mysore, V. (2019). Surgical Smoke in Dermatology: Its Hazards and Management. Journal of Cutaneous and Aesthetic Surgery, 12(1), 1-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6484569
Note: For more information go to STERIS Smoke evacuation system and Surgical Smoke Evacuation Systems In The OR | Knowledge Center (steris.com)
 AORN
AORN.svg?sfvrsn=be606e78_3)



.svg?sfvrsn=56b2f850_5)