There's a lot riding on turning over operating rooms quickly between cases. It ensures high-volume surgeons start their surgeries on time, patients pass through pre-op without delay and the surgical schedule remains packed with profitable procedures. Banner Baywood Medical Center in Mesa, Ariz., has become a model of efficiency since 2016, when the orthopedic service line established a new performance indicator: Surgical staff had to lower their average turnover times from 28 minutes to 22 minutes. Achieving that goal demanded new thinking, a bit of creativity and plenty of teamwork.
- Home
- The Magazine
- Article
Rapid Room Resets
By: Maria Marabito
Published: 12/10/2020
A medical center's ability to slash six minutes off OR turnover times presents a blueprint for success.
Culture change
The medical center's staff members know what roles they play in the turnover process and have bought into efforts to work more efficiently. Surgical techs are in charge of breaking down the back table and disassembling instruments before sending them to sterile processing. Circulating nurses keep the turnover process organized by assigning responsibilities to available team members, so tasks aren't repeated and everything that needs to get done is covered.
"If two people are working on cleaning up and removing garbage, they'll say, 'You take the garbage,' and, 'You go wipe down the anesthesia equipment,'" says Karen Tjelmeland, BSN, RN, CNOR, Banner Baywood's nurse manager. "They delegate roles."
Team members who clean OR surfaces follow AORN's recommendations and cleaning products' guidelines for kill times. Staff receive specialized training related to OR cleaning, which is reviewed and tested annually. An emphasis on teamwork is promoted by removing the presumption of "business as usual," an effort that involves engaging surgeons and anesthesiologists to be part of the process. "The anesthesiologists got onboard with the quicker turnovers," says Ms. Tjelmeland. "They oversee nurse anesthetists, who meet with patients in pre-op to ensure they're ready for surgery as soon as rooms are finished."
Preparing ahead of time also helps the team work efficiently between cases. They participate in daily morning huddles with OR schedulers, the OR manager, supply chain personnel and the sterile processing lead. "During the huddle, we review the schedule to make sure we have no conflicts with requests for equipment, and that we have all necessary instrument trays available for the next day's cases," says Ms. Tjelmeland.
Staff always check their rooms' equipment carts first thing in the morning to see what their needs are and communicate with the sterile processing department about which instruments will be needed to be turned over quickly for upcoming cases. OR assistants anticipate when rooms will ready for cleaning and plan accordingly by, for example, placing mops and buckets outside rooms before cases end. This teamwide organization contributes to keeping efficiency high and room turnover times low.
Active leaders

Banner Baywood's leadership has been very involved and present in improving room turnovers, and worked to remove barriers along the way, including banishing the idea that staff doesn't have enough help. "We needed to change the way they approached their daily work, and that involved first changing their mindset," says Ms. Tjelmeland.
Banner Baywood's leadership also realized early on the importance of being present and visible to staff while they're working. "They've commented on how nice it is to see the manager of our sterile processing department in our ORs, actually talking to the surgeons," says Rosemarie Roesler, MSN, RN, CNOR, CSSM, senior nurse manager.
The involvement of managers in leadership roles is essential to room turnover success. "I think staff, surgeons and anesthesiologists are very comfortable coming to us with any concerns they have, and they know that we will take care of them right away," adds Ms. Roesler. "We don't sit behind closed doors. Everybody is involved."
Because the managers are so visible, they're able to acknowledge and address areas for improvement and implement changes. "We found that turnover times increased at 11 a.m., when most staff members take their lunch breaks," says Ms. Tjelmeland. "Now, when I assign lunch breaks, I make sure a lunchtime turnover team doesn't eat until 12:30. We have designated staff members who don't eat lunch until later, so there are always enough team members available to help turn over rooms."
Leadership also created a "green sheet," which serves as a tool for real-time data collection.
Staff complete the form every day, recording times for when patients exit the OR, when rooms are cleaned and when next patients are wheeled in, with specific notes on why a turnover may have lasted longer than expected.
"We've been able to easily implement good communication practices because we were visible and always talking with physicians and staff," says Karen MacDonald, MSN, RN, CNOR, RNFA, a senior manager at Banner Baywood.
The engaging and open workplace culture is something that has been developed over the past few years. "Our leadership team has been together for four years now," says Ms. Tjelmeland. "We really like to make work a fun, enjoyable place. We're all here to take great care of patients, which involves everybody in the department."
Friendly competitions
Improving turnover times wasn't just a priority of the center's leadership. Staff at Banner Baywood indicated they had the same goal when filling out their annual evaluations. They received points on their evaluations for meeting the 22-minute goal, which gave them extra incentive to decrease turnover times.
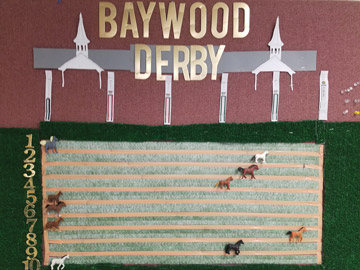
To keep staff motivated and engaged in efforts to turnover rooms faster, leadership turned the process into fun competitions, using games to spark the team's interest. "We correlated the green sheet with some fun activities on our bulletin board in the hallway outside the ORs," says Ms. Tjelmeland.
For example, a Kentucky Derby-themed competition involved assigning ORs to plastic horses, which were moved across lanes on the bulletin board based on the fastest recorded turnover times. Between cases, team members would run to check if they had a fast enough turnover time to make headway in the race. The winning horse was announced at a staff huddle.
Leadership also created a football field bulletin board, on which surgeons' names were written on footballs. To reach the end zone, their OR team had to meet or exceed the established room turnover goal. "Games like this made surgeons and staff excited to do better," says Ms. Tjelmeland.
Widespread adoption
Banner Baywood's leaders speak about their team's accomplishments by emphasizing that implementing change is where the challenge lies. They say it takes commitment from leadership in all areas to own their part in the process, accept the responsibility for their team's role and embrace and support the changes necessary to improve room turnover times. The methods they implemented to improve room turnover times were designed to be easily replicable in other facilities. Instead of isolating the improvements to orthopedic surgery, Banner Baywood's leadership decided to incorporate their methods across the entire hospital and nine other facilities within its health system.
The facility's staff and management are proud of the improvements they made. Change did not happen overnight, however. The effort involved investing time and energy into streamlining processes and channeling patients in and out of the OR in an efficient manner. "It takes a lot of work," says Ms. MacDonald. "We put forth the vision, but we also engaged the team to make it happen." OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)