Management of BPH with prostate-relaxing medications is the first treatment option and is effective in improving symptoms for four to possibly 10 years. However, more than 25% of medically managed patients are noncompliant or discontinue their therapy due to associated side effects such as nasal congestion, dizziness and ejaculatory dysfunction. Plus, the prostate continues to grow, and suffering men will eventually need to undergo surgery when the symptoms become intolerable.
TURP, long considered the gold standard surgical intervention, involves removing segments of the prostate gland with a resectoscope placed through the urethra. TURP procedures are invasive, lead to longer recoveries with increased risk of bleeding and result in longer catheterization. Many men avoid undergoing this procedure due to concerns about long recoveries, complications and side effects, including losing the ability to ejaculate. The procedures are performed in 45 minutes to an hour with the patient under general anesthesia and typically require a minimum 48-hour catheterization after surgery. For that reason, a significant percentage of these procedures can't be done in the outpatient setting.
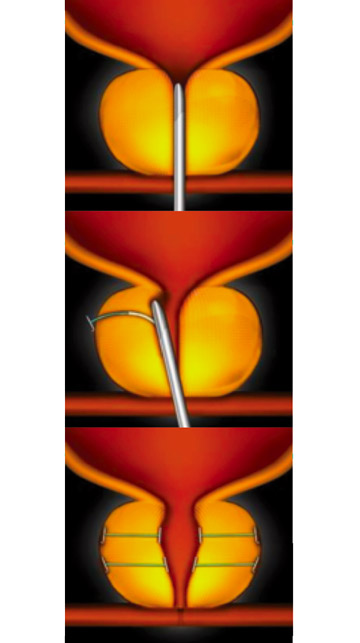
The prostatic urethral lift procedure offers a middle ground between medication therapy and the more invasive TURP. Men who are on medications, but tiring of the associated side effects, can opt to undergo the lift procedure to get off the therapy.
Although the lift isn't quite as effective as TURP in terms of increasing urinary flow rates, patients recover quickly and return to normal life activities within three to five days. Two-thirds of patients don't need to be catheterized after the procedure. Half of my patients with enlarged prostates undergo the TURP procedure and half undergo the lift (I perform about 10 per month). Men with large prostates might require the more invasive TURP procedure, but those with moderate sized or a smaller symptomatic prostate are candidates for the lift procedure. Patients who undergo the lift are not precluded from later TURP if indicated.
The lift is also an appropriate option for patients who aren't candidates for TURP, including older, sicker men in whom anesthesia would be risky or patients for whom holding blood thinners are contraindicated. Unlike the TURP procedure, patients don't have to stop blood thinners before having a lift performed.
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)