On a winter’s evening in 2017, Chris Fuller, MD, was about to cut into the most vibrant green bell pepper he had ever seen. “It was splayed before me, in brilliant 4K high-def glory, on a 55-inch flat screen monitor,” recalls Dr. Fuller, an ophthalmologist at Texas Retina Associates in Fort Worth. He slipped on a pair of 3D glasses and grabbed microsurgical forceps to deftly extract the pepper’s seeds. He was practicing with the new heads-up display in preparation for using it the next morning during an actual surgery. “Since then, I’ve never looked back,” says Dr. Fuller. “I’m a huge champion of the technology.”
During a recent conversation, Dr. Fuller was stunned to learn that his practice was the first in Texas and only the fourth nationwide to use the heads-up technology to perform vitreoretinal surgery. While he says the system is starting to gain momentum with cataract surgeons, he finds it perfectly suited for all of his retinal cases. “It really excels when engaging in detailed, delicate macular (central retina) work,” he explains. “The macula is arguably the most important and irreplaceable structure within the eye, and success — or bloody disaster — is often measured in microns.”
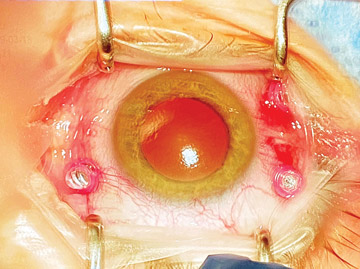
Dr. Fuller says 3D heads-up displays offer unparalleled depth of field that exceeds a surgical microscope at certain aperture settings, high-dynamic-range imaging and an array of switchable color profiles that can be activated to achieve the best possible visualization in a variety of challenging clinical situations. For example, when operating on a patient suffering from dense vitreous hemorrhage, the system allows him to toggle to a “red free” setting, which makes the underlying retina more visible.
“Not only does this speed up surgical times, it enhances patients safety by making surgeons far less likely to clumsily bump against the retina in the fog of surgery,” explains Dr. Fuller.
The brightness of the surgical field can be superior to that of traditional surgery, without exposing the retina to additional light. “I commonly operate at 15% to 20% luminance with heads-up displays, whereas my colleagues who still use microscopes are commonly operating at 50% or higher,” says Dr. Fuller. “Lower illumination settings make rare cases of retinal phototoxicity even far less likely.”
Improved ergonomics are another advantage afforded by heads-up displays. Numerous ophthalmic surgeons struggle with repetitive strain injuries to their backs and necks that are caused by sitting in static positions at a microscope’s oculars for hours on end. “My back still barks at the end of a long day in the OR, but that discomfort has lessened since using this technology,” says Dr. Fuller.
He also thinks the technology’s benefits far outweigh its minor downfalls and significant price tag. “Some surgeons have griped that peripheral retinal visualization is a bit awkward, but most of those concerns melt away after three or four weeks of dedicated 3D use,” says Dr. Fuller. “Also, many surgical facilities are not keen to dump $100,000 on a device that does not directly and immediately increase a facility’s cash flow, especially in these hardscrabble times of COVID-19.”
.svg?sfvrsn=be606e78_3)

.svg?sfvrsn=56b2f850_5)