Getting back up and running and returning to a sense of normalcy are phrases that have been thrown around since COVID-19 hit. As elective procedures such as colonoscopies began to ramp back up after last year's nationwide shutdown, high-volume GI centers had to take a long look at their practices and protocols in order to maintain efficiency and screening success while also making sure patients felt safe. The pandemic threw them a major curve ball, but their physicians and staff quickly pivoted in order to keep scheduling screenings that can save the lives of the more than 100,000 patients who are diagnosed with colon cancer each year.
- Home
- The Magazine
- Article
Colon Cancer Doesn't Wait for COVID-19
By: Danielle Bouchat-Friedman
Published: 1/6/2021
Scheduling colonoscopies during the pandemic requires clear communication, strategic case scheduling and strict safety protocols.
Staying current
Before COVID-19, physicians at the Center for Digestive Health & Nutrition in Moon Township, Pa., performed approximately 7,500 colonoscopies each year. At the beginning of the pandemic, when elective procedures were put on hold and only emergent procedures were being performed, the facility saw an 80% to 90% reduction in its normal screening volume. "We had a horrible two-month dip, so we knew our numbers were going to be low last year," says Frank Kim, MD, a gastroenterology specialist at the center. "And it took some convincing to get patients to return to get the screenings they needed done."
Early on, Dr. Kim experimented with telehealth and was surprised by how much his patients enjoyed the experience. "The patient satisfaction surveys were at 98%," he says.
The National Colorectal Cancer Roundtable (NCCR), a national coalition established by the CDC and the American Cancer Society, says last year's shutdown of elective procedures caused a 90% drop in colonoscopies and biopsies through mid-April 2020, compared with the same period in 2019. As a result, according to the NCCR, more than 18,000 people are now at risk for delayed or missed diagnoses of colorectal cancer and more than 4,500 more people will die from the disease in the next decade.
Michael Sapienza, CEO of Colorectal Cancer Alliance in Washington, D.C., the largest and oldest colorectal cancer nonprofit organization in the U.S., says it is incredibly important for facilities to prioritize screenings for high-risk patients during the pandemic — including those with a family history of colorectal cancer or polyps, or other comorbidities such as Crohn's disease, ulcerative colitis or inflammatory bowel disease.
"Both the Colorectal Cancer Alliance and the American Cancer Society have endorsed screening at age 45 (rather than 50) and now the United States Preventative Task Force has the draft recommendation at 45," says Mr. Sapienza. "We hope they stick with the draft recommendation."
Mr. Sapienza points out Black Americans are twice as likely to get colorectal cancer and four times as likely to die from the disease, so efforts must be made to provide better support, education, awareness and screening options for these patients.
Screening rates are also on the decline because many Americans have lost their jobs and health insurance during the pandemic. To address this issue, the Colorectal Cancer Alliance established a financial assistance program for patients who do not have insurance or who are underinsured. Additionally, the ColonoscopyAssist program, founded in 2010 to remove financial barriers to colorectal cancer screening for the uninsured, offers reduced screening rates.
Congress also just passed the Removing Barriers to Colorectal Cancer Screening Act of ?2020, which modifies cost-sharing requirements for colorectal cancer screenings for Medicare patients. Over the next 10 years, the bill will waive coinsurance requirements for screening tests, regardless of whether a polyp is discovered and removed. Currently, Medicare beneficiaries must pay a 20% copay if a polyp is excised during a scheduled screening.
Mr. Sapienza emphasizes that the best test for colorectal cancer is the test that gets done. So, if patients are still wary of in-person screenings during the pandemic, he recommends at-home stool tests.
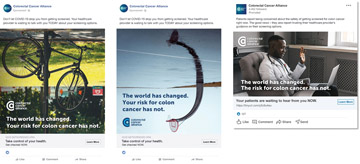
Patients must clearly understand the importance of getting screened, even during the pandemic, according to Mr. Sapienza. He says, "We're running a public awareness campaign right now that notes things are different, but the risk for colorectal cancer is not, so patients need to get screened now."
For added protection, the facility took the necessary safety precautions, including social distancing and allowing only one patient in the waiting room at a time. They also installed acrylic intubation boxes, which have two holes drilled in the back for the nurse anesthetist and another on the side at a 90-degree angle through which the physician manuevers endoscopes during upper GI exams.
Dr. Kim admits it's hard to make his patients feel safe when safety guidelines are rapidly changing. Just days before Thanksgiving, Pennsylvania announced that anyone traveling outside the state had to quarantine for 14 days or have a negative COVID-19 test within 72 hours of their appointment. "Luckily, we have an intake manager who stays on top of these guidelines to keep staff and patients informed," he says.
Due to the constant changes in local pandemic response protocols, Dr. Kim makes sure his staff and patients are aware of the safety precautions in place at the facility. He says his center's website is frequently updated to reflect that it is 100% compliant with the state's protocols.
Dr. Kim says clear two-way communication with patients is essential. The facility set up an intake management system where patients can submit needed information before procedures, so patients spend as little time as possible filling out paperwork on the day of their procedures. Additionally, patients' drivers stay in their cars and receive text message updates when procedures are done. "We coordinate having the minimum number of people in the center, and it actually works quite well," says Dr. Kim.
Laura Young, RN, director of nursing at Greenwood (S.C.) Endoscopy Center, says advertising their safety measures was key to getting their facility back up and running. "We let our patients know that their temperatures will be taken upon arrival and that they will be asked about travel and upper respiratory symptoms," she says. "If they have traveled or are positive for symptoms, their appointment will be rescheduled. ?Anyone accompanying a patient during their appointment must wait in their vehicle to limit the number of people in the waiting area. All patients and staff are required to wear masks while in the center."
Ms. Young believes you cannot overemphasize the importance of patient education, especially during a pandemic. "We provide patients with handouts on our policies and the screenings they undergo, and we call patients the day after their procedures to check on them and answer any questions they may have," she says. "We also make it a priority to get the word out in the community about the importance of colonoscopy through local news outlets."
Smart scheduling

Before COVID-19, it wasn't uncommon for Dr. Kim to schedule screenings months in advance. He schedules more cautiously these days. "We had to cancel 200 cases when the pandemic hit, which was difficult to do," he says. "When we first opened back up, we took it month by month."
There is an art to scheduling cases effectively and efficiently, especially following a pandemic. You must factor in the procedure being performed, sedation and recovery times, as well as room turnovers, which take longer due to the extra cleaning regimens in place during COVID-19. In order to perform an average of 50 screenings a day, Dr. Kim hired extra staff to help disinfect and turn over rooms.
Dr. Kim says the center takes more precautions before appointments to help prevent case cancellations and scheduling issues. For example, the facility calls patients two to four days prior to their appointments, and patients are required to fill out a COVID-19 questionnaire before intake. The goal is to keep the case schedule filled, but safety is more important. "If patients don't comply with the regulations we have in place and we have to cancel cases, we will," says Dr. Kim.
Ms. Young says minimizing pre- and post-procedure inefficiencies can help free up time to focus on procedures. "For example, we have all patients come into the clinic for a pre-procedure work-up," she explains. "Lots of information gathering and teaching occurs, and that's when we have patients sign insurance and consent forms."
The facility's staff also previews the next day's procedure schedule and will move the start time of cases up in order to fill gaps and decrease wasted time.
Positive reviews
Dr. Kim appreciates how quickly his patients have adapted to the facility's new processes and, in turn, they appreciate the extra mile his center has gone to keep them safe. "Patients recognize the safe care we've been providing," he says. "They tell their family members and friends. They know we'll do whatever it takes to perform procedures safely."
Word travels quickly, leading to more essential screenings being performed — even during the pandemic. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)