For the second straight year, outpatient surgery leaders were forced to work in extremely difficult conditions. Not only did you continue to fight the scourge of COVID-19 by protecting yourselves, your staffs and your patients, but unprecedented
staffing shortages have forced some of you to don surgical attire and work in ORs far more than you envisioned.
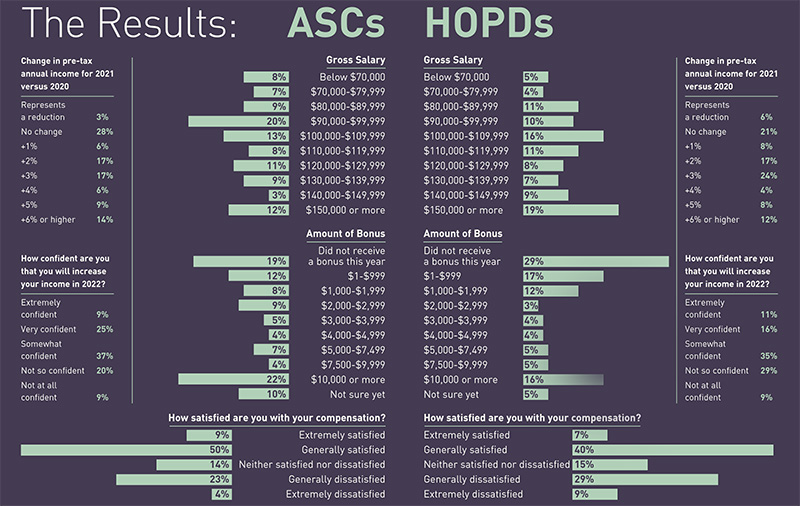
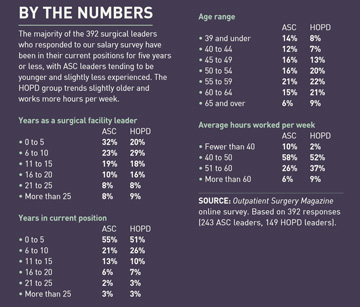
While 59% of the 243 ASC administrators and 48% of the 149 HOPD leaders who responded to our annual salary survey reported being happy with their compensation, some wondered if what is currently considered industry-average pay really
accounts for the stark increase in the amount of work they must do — and the different roles they need to fill expertly at the drop of a hat. Our survey revealed high levels of exhaustion and extremely full plates for many of you —
yet also, a signature dose of optimism and satisfaction. Let’s dive deeper into what you had to say about your compensation after another eventful year filled with plenty of stress and inspiring success.
- Home
- The Magazine
- Article
Your Plates Are Full
By: Joe Paone | Senior Editor
Published: 1/5/2022
Outpatient surgery leaders are paid well, but some wonder if their salaries meet the level of the expanding responsibilities they’re managing during the ongoing pandemic.
Heavy load

An overwhelming 86% of ASC leaders and 85% of HOPD leaders say the volume of their work responsibilities has increased over the past 12 months. The reasons, however, vary. On the HOPD side, being part of a hospital system inflicted serious COVID-related stressors on leaders. Administrators at ASCs grappled with shutdowns, facility expansions, staffing issues, tech upgrades and additional job responsibilities on top of everything they were already doing.
Cori Grice, RN, director of nursing (DON) at Knights-bridge Surgery Center in Columbus, Ohio, says she’s taken on new responsibilities over the past two years. “I was brand new to this role when I was hired in February 2020,” she says. “As a new DON, I had to learn how to close a center down, reopen the center, and write and implement the necessary policies and procedures surrounding the pandemic. Before 2020, my role didn’t have the weight of that kind of responsibility. We’re now expected to be CDC and COVID experts, which, as we all know, is ever-changing by the day.”
Compounding that issue for Ms. Grice have been unpredictable staffing challenges related to the pandemic. “Staff members who call off because they aren’t feeling well often need a COVID test before returning to work, which could take up to four days,” she says. “A staff member could also call off because a family member isn’t feeling well or their child is in quarantine due to a possible exposure at school. Before the pandemic, the call-offs were few and far between. Now, when a nurse is out, I tend to fill their role for the day.”
Ms. Grice says this constant bouncing between administrative and clinical roles is draining. “Most of the time, I am having to fulfill my managerial role and a staff role at the same time,” she explains. “This can be stressful and overwhelming, which ends up with me being exhausted by the end of the day.”
Still, she sees positives amid the stress and uncertainty. “I’m thankful I can be versatile in my managerial role, and still connect with my staff and work next to them,” she says. “I have a great team that helps and supports each other, and we work well as a unit. I also have an amazing family that loves and supports me when I come home stressed or rundown. Without my great team at work, my husband and kids, I would be more stressed than I currently am.”
Dedicated, dutiful and versatile surgical leaders continue to put their heads down and power through the challenges of their daily responsibilities. “We do whatever needs doing,” says Suzi Cunning-ham, administrator at Advanced Ambulatory Surgery Center in Redlands, Calif. “And if we haven’t done it before, we learn how to do it.”
HOPD leaders, on the other hand, have increasingly been funneled into helping their overtaxed parent hospitals continue to function, as massive amounts of staff have been called into the ongoing emergency of treating an incessant flow of COVID-19 patients — all while persistent staff attrition increases the pressure and workload on everyone who’s left behind.
“I’ve had to cover all the areas of surgical services — pre-op, PACU, endoscopy, pre-admission testing and sterile processing,” says Jacqueline Cabrales, MHA, BSN, RN, CNOR, CSPM, director of surgical services at Fort Duncan Regional Medical Center in Eagle Pass, Texas. “I take call on the weekends so that PACU nurses can rest. Some weeks, they’re on call five out of seven days. I’m blessed to be a well-rounded provider. Being able to assist the staff has truly helped the entire team.”
Two-thirds (66%) of HOPD leaders say they’re burned out at their jobs, compared to about half (52%) of ASC administrators. Given the two-pronged wallop of an unpredictable pandemic entering its third year and an increasingly precarious staffing situation that is impacting daily workflows and effective patient care, it’s not surprising that many surgical leaders are worn down to a nub.
Laura Picano-Wilson, RN, CNOR, CAIP, clinical director at Livonia (Mich.) Outpatient Surgery Center, believes her compensation is fair but still feels the effects of burnout, which she says is typical of the fourth quarter in any year due to the deductible-driven rush among patients to have elective surgeries before year’s end. “Surgeons and management want the numbers and patients want the procedures completed, so the workload is intense,” she says. “I have learned to concentrate on what I can control, continue practicing self-care and take some days off so I can return refreshed after the holidays are over.”
Ms. Picano-Wilson is another leader who talks about the head-spinning nature of her job in the pandemic era. “Some days it’s hard to switch gears from clinical to administrative responsibilities, but I prioritize and complete what I can at the moment before moving on to the next challenge,” she says. “I’ve always been involved with patient care on most surgical days to keep cases moving along. It can be hard to juggle at times, but I arrive early to take care of emails and use my evenings and down time for admin responsibilities.”
Staffing issues have made it difficult for Ms. Picano-Wilson to settle into a leadership routine. “Most hospitals are offering wages and guaranteed hours that we cannot promise or afford,” she says of her ASC. “Surgical volume has been unpredictable, making it hard to decide what positions are needed and sustainable.”
She focuses on keeping the dedicated staff she already has happy. “Most of my employees have been with us for many years, so we spoil them with bagels or lunches any chance we get,” she says. “I’m hopeful 2022 will be a better year for us all.”
Denise Latimer-Wright, RN, CNOR, clinical director at Lakeview Surgery Center in Bowie, Md., configured and implemented an EMR over a three-month period, then jumped to coordinating an expansion project that doubled her facility’s space. She was primarily responsible for procuring capital equipment and coordinating electrical, plumbing and medical gas work on weekends and off hours because the center remained open during the remodeling.
“I haven’t been able to take time off because I’ve had to be present to coordinate so many projects,” she says. “There’s no one currently capable of being in charge in my absence — efforts to recruit a charge nurse have been unsuccessful. The expansion also resulted in me having to recruit, hire and onboard additional staff and credential new medical providers. It’s been one thing after another, and it never seems to end.”
Pay vs. responsibility

The majority of the survey’s respondents feel they’re well-compensated, but some believe they could be earning more based on the number of hours they work and the many aspects of surgical care they manage. Rachel Piszczek, BSN, RN, CNOR, CAPA, CNAMB, CSSM, director of perioperative services at The Surgery Center of Fairbanks in Alaska, feels she is paid the average for someone in her position and with her experience. “However, if my rate was calculated for hourly pay rather than an annual salary, I’m grossly underpaid for the amount of time I put in,” she says.
Inappropriate compensation in light of workload and responsibilities was a recurring theme among the survey responses. “I’m similarly paid to clinical nurses and I have more total years of experience, so that is a little disappointing for my management responsibilities,” says Barbara Monroe, pre-op/PACU supervisor at Tuscon (Ariz.) Surgery Center.
The lion’s share of responses reflected frustration with workloads. Ms. Grice feels that the DON position, especially during the pandemic, is undervalued. “We have many responsibilities, even working from home on weekends, that we are not compensated for,” she says.
Some HOPD leaders also feel their pay doesn’t align with their responsibilities. “My facility has given bonuses, raises and other incentives to frontline nurses, but not to those who managed the many changes over the last year,” says Amanda Brady, clinical director at Luminis Health Anne Arundel Medical Center in Annapolis, Md.
“Given the increasing challenges of managing the variables of an OR environment, industry compensation has been focused on frontline staff — which is a good thing — at the expense of compressing leadership compensation,” says Frank Sciolini, director of surgical services at Ascension Saint Thomas in Nashville, Tenn. “The unintended consequences have been more responsibilities with less compensation that creates a challenging environment to recruit and retain surgical supervisors. This is now leading to more inexperienced leaders filling leadership roles.”
Brian Bizub, BSHA, executive director and CEO at Raleigh (N.C.) Orthopaedic Clinic, has spent much of the last two years managing significant company growth while juggling endless pandemic-related issues. His ASC, which opened in 2013, is performing more joint replacements than ever before, even after a month-long shutdown during the height of the pandemic. In fact, 2020 was his facility’s biggest volume year ever at 7,000 surgical cases, and it performed just a bit fewer — but still more than 6,500 — in 2021. A focus on safety and trends in the local population kept his service lines humming.
“We put a lot of measures in place to ensure our staff and patients were safe,” says Mr. Bizub, who believes remote working freed up time and resources for many patients to get the elective surgeries for which they might not have had time for in the past. “I think people who were putting off surgery because of having to take time off from work were able to go ahead and schedule their surgeries,” he says.
While the pandemic has made some patients hesitant to go to acute care hospitals for care, Mr. Bizub believes it also presented a great opportunity for outpatient facilities. “Rehabbing is much easier at home than it is at a workplace, so people were able to have surgery and still continue to work without taking several weeks off to recover,” he says.
One of Mr. Bizub’s biggest challenges has been managing robust flows of patients during a national staffing crisis. He says his ASC is getting by thus far, although he’s actively recruiting new providers.
“We treat our employees well and value them, but some of the market forces are difficult to compete with,” says Mr. Bizub, who notes that many qualified employees have been seeking higher paydays as travel nurses, who earn $20 an hour or more than what his surgery center can pay. He’s seen travel nurse positions that pay $4,000 a week with generous stipends for traveling and living expenses.
“Some nurses will try to make as much money as they can until things settle down, and then look for full-time employment,” he says.
Mr. Bizub opened a second ASC last year and secured a certificate of need for a third facility that will be constructed in 2024. He guided his center through two successful accreditation surveys. He’s keeping tabs on population growth in North Carolina and strategizes to position his center for future growth, and spends time recruiting surgeons.
“I’ve been in the hospital world, so the stress is a little different there than it is here,” he says. “Some days are challenging, and other days everything runs very smoothly and it’s not such an issue. But the hours are long.”
At the end of another grueling day, Mr. Bizub, like so many of you, still loves his job.
“My staff is excellent with patients, and they work together as a terrific team,” says Samantha Dillon, administrator/director of nursing at Desert Endoscopy Center in Mesa, Ariz. “Being able to work alongside such amazing people is rewarding and keeps me motivated to make my center the best it can be.”
Bobbi Freeman, RN, MSN, CGRN, ASC administrator and practice manager at Harbin Clinic Gastroenterology and GI Lab in Rome, Ga., believes the benefits of her job can’t be fully accounted for in her paychecks. “I pride myself on being a good leader, a great nurse and a role model for my team,” she says. “I do everything in my power to make it easy for my staff to take care for patients. When I leave work every day, I know I made a difference. That makes it all worth it.” OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)