Reprocessing flexible endoscopes is a never-ending job filled with potential pitfalls that can jeopardize patient safety. Our endoscopy center performs about 60 cases a day, so our facility’s fleet of more than two dozen scopes needs to be reprocessed quickly and effectively. Despite the time crunch, we never cut corners during the multi-step process and haven’t had a single patient infection during the nine years I’ve been working here.
Our well-oiled reprocessing machine begins at the bedside. After a procedure is finished, the nurse in the room precleans the scope. They use a detergent that’s diluted with water, so there’s a formula they need to follow. Generally, the process takes two to three minutes. We use rigid containers to transport the scopes to the decontamination area, which is adjacent to the procedure room. Because scopes are moved a short distance through a single door, we didn’t invest in medical-grade transport containers; we simply purchased clear plastic totes whose lids fit the size of our scopes perfectly when they’re wound. They are disinfected after each use.
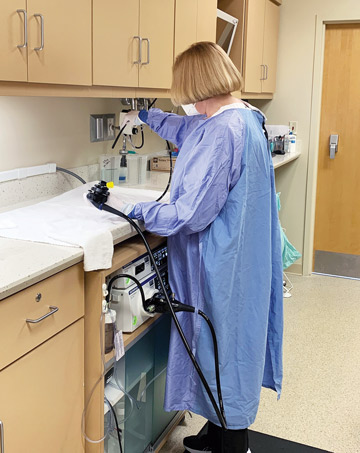
Once scopes are in the hands of reprocessing techs, leak-testing is done, which takes a few minutes. Techs place a scope in a sink full of clean water and connect it to a wall-mounted leak tester. Next, techs do a manual cleaning in the sink, wiping off the insertion tube, checking all the channels and inserting cleaning brushes through them.
After they hook the scope to a device that flushes the channels, it’s ready for a 26-minute high-level disinfection cycle in our automated endoscope reprocessor (AER). Toward the end of the cycle, the scope is flushed with water and alcohol, and then air for drying. When the cycle finishes, a tech brings the scope to our clean equipment room, dries residual fluid on the outside with a lint-free cloth, and hangs it in a storage cabinet that meets the appropriate ventilation requirement for next use. In addition to clean scopes, we also store dilators for upper endoscopies, guide wires and cautery devices. We also keep a couple older scopes around as backups and reprocess them every seven days.
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)