Make the most of this common teachable moment.
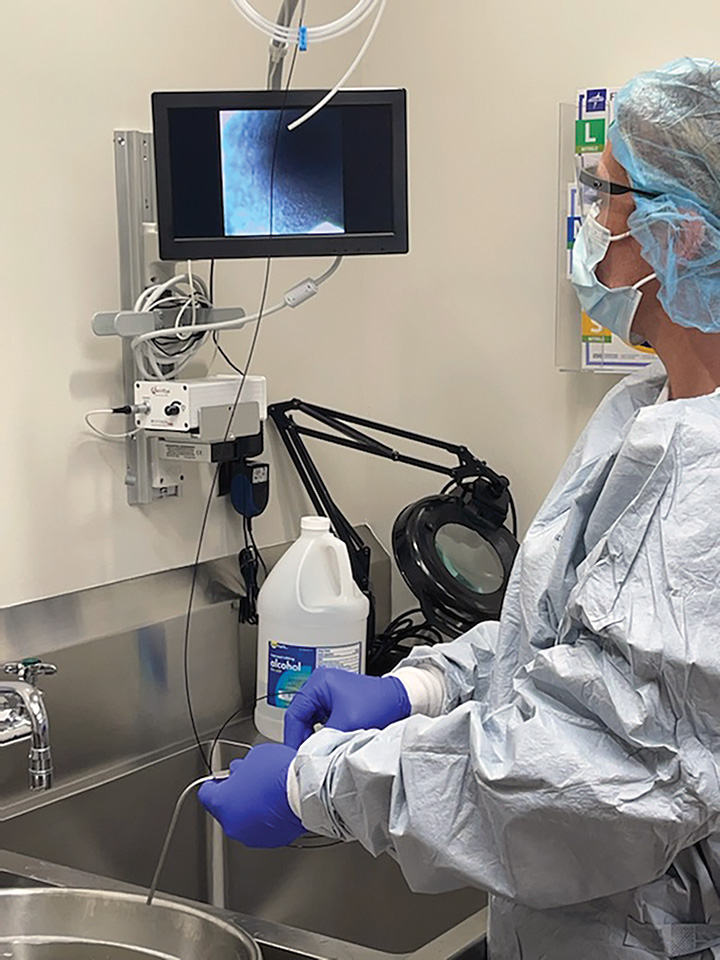
 HEAD START By precleaning instruments to remove bioburden before it hardens, OR staff make manual cleaning quicker and easier for sterile processing techs while better ensuring full sterilization.
HEAD START By precleaning instruments to remove bioburden before it hardens, OR staff make manual cleaning quicker and easier for sterile processing techs while better ensuring full sterilization.
Organic matter is discovered on critical, regularly used instruments. Do you: a.) Ask sterile processing what happened, or b.) Reach out to your surgical techs to learn if precleaning was missed among their laundry list of tasks, and then reiterate the importance of this crucial but too-often neglected practice?
If you answered "b", Frank Myers, MA, CIC, FAPIC, assistant associate director of infection prevention and clinical epidemiology at University of California, San Diego Health, appreciates your knowledge and understanding of the full scope of instrument cleaning. Mr. Myers has seen sterile processing departments take the blame on many occasions for a missed step in the instrument cleaning process that truthfully is the responsibility of surgical techs.
When this happens, Mr. Myers suggests taking a step back and using it as a teachable moment, as it’s a prime opportunity to revisit communication between the sterile processing department and the OR. When organic material is discovered in sterile processing, he says, institutional leaders should first reach out to surgical techs. Such discussions also provide great opportunities to uncover workflow issues.
"You need to have a discussion with your techs and find out how the precleaning is missed," says Mr. Myers. "Maybe it’s just ignorance or not knowing, but maybe there’s a bigger issue. Maybe the techs are multitasking too much and need to let leadership know, "I’m running three ORs and…’"
Regardless of whether any major changes are made, investigating these problems provides you another opportunity to reiterate the absolutely essential importance of precleaning. "One of the most basic tenets of instrument care is making sure precleaning takes place at the bedside by OR staff," says Mr. Myers. "They should be removing gross debris and organic matter in the OR, and the instruments should be wet when they make it back to the sterile processing department."
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)