- Home
- Special Editions
- Article
Reader Survey on Patient Warming
By: Jared Bilski | Editor-in-Chief
Published: 4/29/2025
What your peers are doing to prevent hypothermia — and why they’re doing it.
Trusted associations strongly recommend warming patients throughout the perioperative process and an array of studies highlight the multiple benefits of this critical process, but what do surgical facility leaders — and their teams in the trenches — think about it?
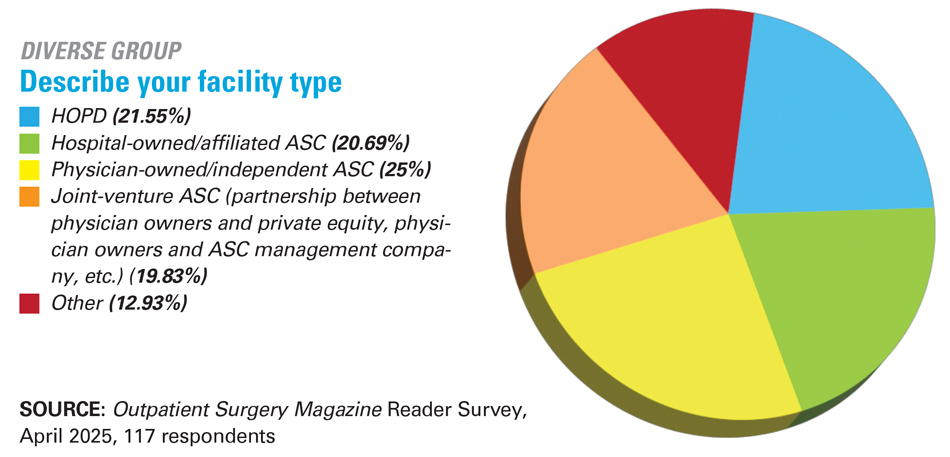
That’s what we set out to uncover with our 2025 Patient Warming Survey, which dove deeply into the who, what, when, why and how of this practice and garnered 117 responses from Outpatient Surgery Magazine readers. Our survey looked at whether outpatient facilities warm their patients, when they do it (pre-, intra-, postoperatively), which warming devices they use, and why they use them. It also gauged how this patient-focused protocol impacts surgical outcomes.
Readers’ responses made one thing abundantly clear: Patient warming is a top priority for outpatient facilities, regardless of their makeup.
‘Always’ by a longshot
Generally speaking, the majority of facilities do warm patients in some capacity. Well over half (62.54%) of respondents from the survey said they always warm surgical patients, which is right in line with the 63% who responded this way to our 2019 patient warming survey. When you factor in facilities that sometimes or occasionally warm their patients, virtually all HOPDs and ASCs have some type of patient warming protocol in place. Specifically, 97.44% of facilities said they warm patients at least occasionally, a sizeable bump from the 90.1% who responded this way in 2019.
When are patients warmed?

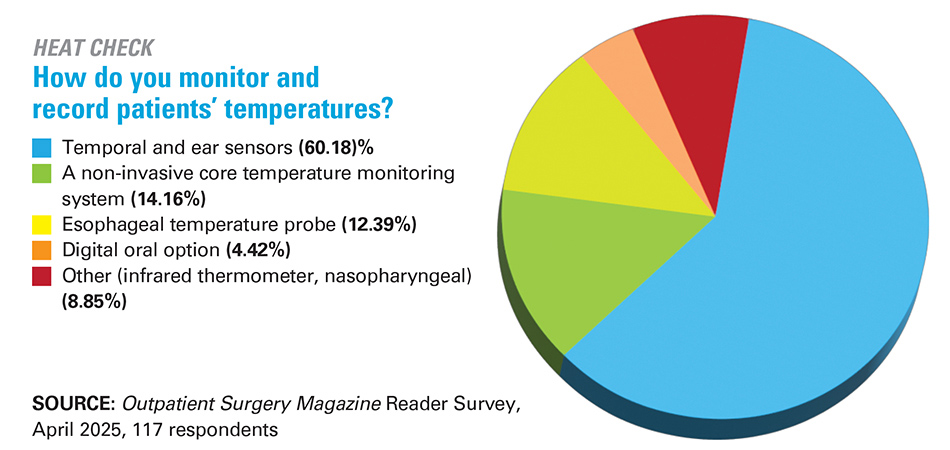
Ideally, patient warming is something that takes place throughout the entire perioperative journey, beginning preoperatively, continuing through the intraoperative phase of care and holding steady postoperatively until discharge. We asked respondents during which phases of perioperative care they warm patients, with the option to list all perioperative phases that apply. Unsurprisingly, 95.61% of respondents warm their patients intraoperatively. But many facilities also employ this critical practice preoperatively and postoperatively, as well. Specifically, 67.54% of respondents employ preoperative or prewarming measures, and 70.18% do so postoperatively. Both represent a slight dip from our 2019 survey (68.8% and 72.1%, respectively.)
There were also a handful of respondents (7.89%) who employ warming measures on a patient-specific basis, such as postoperatively when the patient is hypothermic or when the patient is shivering or complains of being cold.
While more than half of respondents (57.89%) said they warm all patients regardless of the case, there were plenty of facilities that based their warming practices on a variety of factors. For instance, 47.37% said the duration of the surgery was a factor in whether to warm patients, 45.61% said the procedure itself was an important consideration and 35.09% said the type of anesthesia played a role. Interestingly, 20.18% of respondents said the individual patient’s anxiety level plays a role in the warming decision.
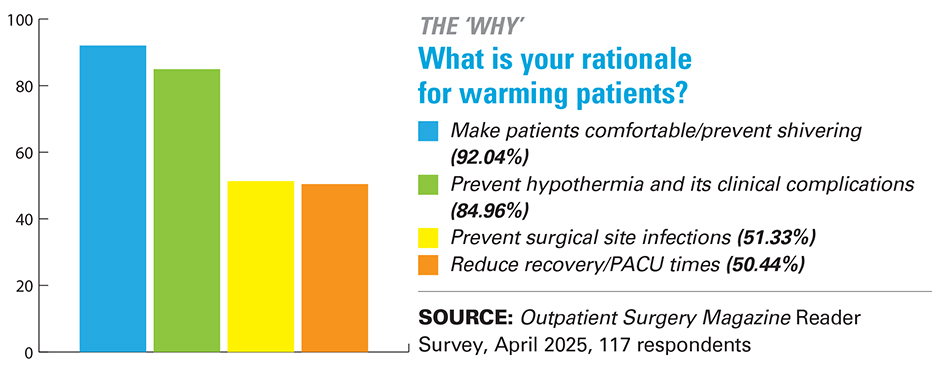
What methods are they using — and why?
Much like in 2019, our latest survey found that facilities predominantly use two main methods to keep patients warm and comfortable: a forced-air warming system (cited by 90.35% of respondents and up from 83.2% in 2019) and/or a cotton blanket prewarmed with a blanket warmer (cited by 82.46% of respondents, compared to the 81.4% who did so in our 2019 survey.)
Other warming methods used by respondents: 8.77% use a spinal underbody blanket (or thermal mattress or bed pad on which the patient lies); 4.39% use some type of radiant warming device; and just 1.75% use a conductive polymer fabric that warms the patient from above and below simultaneously.
When it comes to selecting warming devices, it’s no surprise that price (cited by 40.71%) plays a pivotal role in the decision-making process. However, the top reason facilities gave for selecting a certain product was the reputation of the device/company, cited by an impressive 49.56% of respondents. Vendor recommendations and advertisements were also included as motivating reasons, by 7.96% and 3.54% of respondents, respectively.
A significant group of respondents (30.97%) listed “other” when answering this question. Their write-in responses included “staff preference and experience,” “they [the devices] were here when I got here,” “research and product evaluation,” “patient need” and that the purchase was ultimately an “anesthesia-driven decision.”
Tracking results
There’s no doubt that warm patients equal safe, comfortable patients, which impacts facilities in positive ways such as higher satisfaction survey scores. Feeling warm and comfortable is the type of care that patients remember long after they leave your facility. As Melissa Bogaski, RN, BSN, director of nursing for The Ambulatory Surgery Center at St. Mary in Langhorne, Pa., puts it: “Patients rave about the warm blankets received in pre- and post-op areas, and specifically love when they’re given a fresh warmed blanket in the OR before going to sleep.” Multiple respondents cited improved satisfaction scores — often with glowing comments about the lengths facilities would go to in an effort to keep patients warm and comfortable — as a direct benefit of their facilities’ warming protocols.
Happy patients are enough to make warming a priority. But from the provider perspective, are there any tangible, direct economic and clinical benefits inherent in patient warming? Respondents to the survey sure think so. An impressive 86.49% responded to the question, “Do you believe that warming patients has economic as well as clinical benefits?” in the affirmative, compared to just 13.51% who said, “No.”
In terms of the specific benefits, Mary Pat Bugaj, MBA, BSN, chief nurse for surgery/invasive procedures at VA Northeast Ohio Healthcare System in Cleveland, says patient warming “shortens the length of stay in the PACU and [provides] effective pain management and better hyperglycemic control.”
A director at a facility in the Northeast says that “patient normothermia with 15 minutes post-op is typically above 98%” because of the facility’s patient warming efforts. David Lorenson, PhD, RN, surgical services manager at Aspirus Iron River (Mich.) Hospital, reports improved efficiency and patient satisfaction and reduced pain due to patient warming. From an economic standpoint, Dr. Lorenson offers a simple formula that facilities should keep in mind to measure the success of their warming efforts: “Less complications equal less cost,” he says.
Surgical facility leaders simply can’t overemphasize the importance of keeping patients comfortable throughout their surgical journey — especially during that extra-vulnerable time period when they wake up in the PACU.
That’s why one comment from a leader who endured an unpleasant experience on the other side of the table really strikes a chord.
“You can achieve patient comfort, satisfaction and prevention of adverse effects of hypothermia with minimal economic impact,” says Amy Hunt, RN, clinical director of Ascent Surgery Center in Canton, Ohio. “Speaking from someone who has had multiple procedures and has woken up with such violent shaking that it caused physical pain — it is well worth the cost.”
Dr. Lorenson sums it all up succinctly with just five words: “Perioperative patient warming is imperative!” OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)