Technological advancements have allowed for the gradual shift of complex surgeries from acute care hospitals to outpatient ORs. Several procedures are on the move again, this time to office-based procedure rooms, thanks to minimally invasive approaches, improved pain control options and progressive surgeons who want to provide patients with convenient, effective care.
- Home
- The Magazine
- Article
Office-based Procedures Growing in Popularity
By: Adam Taylor
Published: 4/16/2020
The evolution of surgical care continues as cases move on from the OR.
1. Balloon sinuplasty
This minimally invasive procedure can be safely performed as an office-based procedure, according to Mani Zadeh, MD, FACS, a Los Angeles-based ENT surgeon. Dr. Zadeh estimates that at least half of the balloon sinuplasties performed nationally now take place in doctors' offices. "It's a procedure for which general anesthesia is not required," says Dr. Zadeh. "We can use local or topical anesthetics that greatly minimize any discomfort."
The procedure treats sinusitis by widening the sinus drainage cavity to six millimeters. A deflated or compressed balloon is inserted into the narrow portion of the patient's sinus. When inflated, it essentially squeezes and crushes the soft tissue and creates microfractures in the nearby bone to widen the cavity.
Performing the procedure in the office has multiple benefits for patients. First, they don't have to undergo general anesthesia. Because of that, the recovery is quick. They're awake for the entirely of the operation — the worst post-op symptom is often the feeling of having a stuffy nose — so they can drive themselves home. Patients also avoid the time-consuming admissions process at a hospital or surgery center, and they can skip the pre-op blood test that's part of the evaluation to determine if they're a safe candidate for general anesthesia.
The local anesthetics used for balloon sinuplasties have improved in the last two years, after the operation had begun to move to procedure room, which makes it even more suitable for the office setting. Dr. Zadeh says he used to use common topical sprays or local injectable anesthetics. Now, he partners with compounding pharmacies to increase the concentration of tetracaine, which is commonly used at a lower strength in eye procedures, to 6% in the local anesthetic he uses, making it effective in sinus surgeries. Further, the higher-dose tetracaine used to come in a liquid that tended to drip to the back of the throat. Now it's delivered in a paste form that makes its coverage more precise and effective. "These two simple improvements have made a tremendous difference," says Dr. Zadeh.
Office-based sinuplasty won't work for patients whose nasal pathways are too narrow, however. Surgeons determine the width of the nasal passage preoperatively with an imaging test or during the pre-op evaluation by inserting a thin metallic rod with a camera on the end and a light at the tip in the nose. If that tool, which is used to locate the part of the sinus cavity that is narrowed and clogged, can fit into the patient, that almost always means the balloon will fit as well.
"At this point, the only reason for this procedure to be done in an OR is if the patient simply cannot tolerate the pain of having anything inserted in their nose, or if the sinuplasty is being done concurrently with another ENT procedure," says Dr. Zadeh.
Other sinus procedures are making their way to the office as well. For example, says Dr. Zadeh, a septoplasty balloon has been manufactured for correcting deviated septums as an alternative to the traditional surgery that requires an incision.
2. Prostatic urethral lift
This procedure is seen as a possible replacement for transurethral resections of the prostate (TURP), the main surgical intervention for men who have benign prostatic hyperplasia (BPH). The condition is common — 50% of men in their 50s have it, as do more than 90% of those 80 and older.
Many men with BPH get it treated due to quality-of-life issues, including difficulty urinating, having to urinate many times throughout the night and incontinence. If allowed to progress untreated, serious medical conditions from an enlarged prostate can occur, including retrograde ejaculation, bladder failure and kidney damage.
The prostatic ?urethral lift ?is popular with patients who don't want to experience the side effects of other therapies. Medications that relax the prostate, for example, can lead to sexual dysfunction and don't stop the prostate from growing, so a surgical intervention will be needed at some point. Some men who have undergone the invasive TURP lose the ability to ejaculate.
The prostatic ?urethral lift ?can be performed in an office-based setting because it takes approximately 10 minutes to perform, compared to an hour for a TURP. The TURP also requires a two-day post-operative catheterization, which requires hospitalization.
The admission-to-discharge time for prostatic ?urethral lifts can be as short as an hour. Unlike the TURP, prostatic ?urethral lifts are performed with the patient receiving oral or conscious sedation, usually nitrous oxide and/or a local anesthetic.
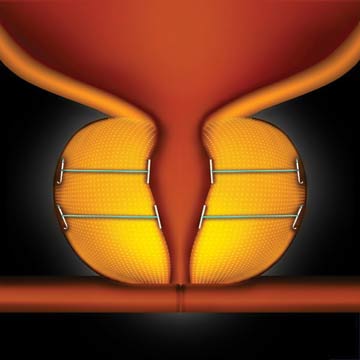
No tissue is removed during the minimally invasive cystoscopic procedure. A rigid cystoscope is inserted into the blocked urethra to gain access to the enlarged prostate. Tiny polypropylene implants are implanted to separate the two enlarged prostate lobes. At least one set of implants is needed, but most procedures require four or six (two or three on each side).
"I'm thrilled to be able to give patients more than a choice between a pill and a TURP," says Peter Walter, MD, FACS, of Western New York Urology Associates. Dr. Walter has performed the procedure more than 650 times. The procedure is popular in part because it doesn't negatively impact the ability to achieve or maintain erections or ejaculate.

"One of the really nice aspects about this procedure is we can get most of patients off medications that have significant side effects," says Dr. Walter. "Often, the adverse effects of medications, especially when patients are taking several, aren't known until years after they've been taking them."
Dr. Walter underwent a prostatic ?urethral lift ?before performing the procedure himself. "I was in my early 50s and started having some symptoms of BPH," he says. "Knowing what I know about the medications and the TURP, I knew I didn't want any part of either of those."
3. Options in eye
Fifty years ago, cataract surgeries were done in hospitals. Forty years ago, they began to transition to hospital outpatient departments. Thirty years ago, their movement into free-standing ambulatory surgery centers. Now, office suites are popping up across the country that could make office-based cataract surgery the next big thing in eye surgery.
"For the most part they are still done in the operating room, but there are some doctors who are part of a new trend who are performing cataract surgery in their offices," says Eric Donnenfeld, MD, a cataract specialist in Long Island, New York. "There is a movement there."
Pterygium surgery is another noninvasive eye procedure that could be a good candidate for the office, according to Amy VanDenBrook, MD, an ophthalmologist with Rosin EyeCare in Chicago. The operation to remove noncancerous conjunctiva growths from the eye takes less than an hour to perform. The biggest barrier for making pterygium surgery work in office settings is pain control, which is easier to control in an OR.
"If IV anesthesia or a retrobulbar block were needed, you obviously couldn't be in a procedure room," says Dr. VanDenBrook.
Minimally invasive glaucoma surgery (MIGS) is often done in conjunction with cataract surgery, but not always. One MIGS procedure, micropulse diode laser treatments, could potentially grow into a common office-based procedure, according to Dr. VanDenBrook. The operation involves delivering a micro pulse of energy to the ciliary body to decrease aqueous production.
"That would be a pretty easy transition because you're technically not going into the eye," she says. "It would be a good fit for a potential migration to a procedure room." OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)