- Home
- The Magazine
- Article
Seamless Sharps Safety
By: Jared Bilski | Editor-in-Chief
Published: 5/8/2025
Here’s help creating a multipronged process that keeps staff out of harm’s way.
The “important part” of the surgery is over, and the sense of relief in the OR is palpable. You can feel the collective exhale of a group that was so laser-focused on the case at hand they needed to occasionally remind themselves to breathe. There’s a noticeable shift in the intensity as wound closure begins and staff’s thoughts meander toward what’s next — the next procedure, the next break, the next case.
Then it happens.
A well-executed surgical case is marred by a sharps injury that could’ve been avoided.
“Between closing counts, surgery ending, emergence from anesthesia and discharge from the OR to PACU, wound closure is a particularly vulnerable time due to the many competing priorities that occur,” says Barbara L. DiTullio, DNP, RN, MA, CNOR, NEA-BC, senior clinical director of perioperative safety, quality and compliance at Beth Israel Deaconess Medical Center in Boston.
Specifically, Dr. DiTullio points to situations where one person takes over the field from another — usually someone who may be less familiar with the team, the procedure and all that has happened during the case — as a prime time for problems. “While staff relief is extremely important and often difficult to manage, recognizing the vulnerability at this time is important in preventing injury and also preventing gaps in communication critical to maintaining patient safety,” she says.
Dr. DiTullio understands the nuance needed to keep staff out of harm’s way. She recently sat down with Outpatient Surgery Magazine to share the essential elements of an effective sharps safety policy as well as helpful tactics to ensure staff stick to it.
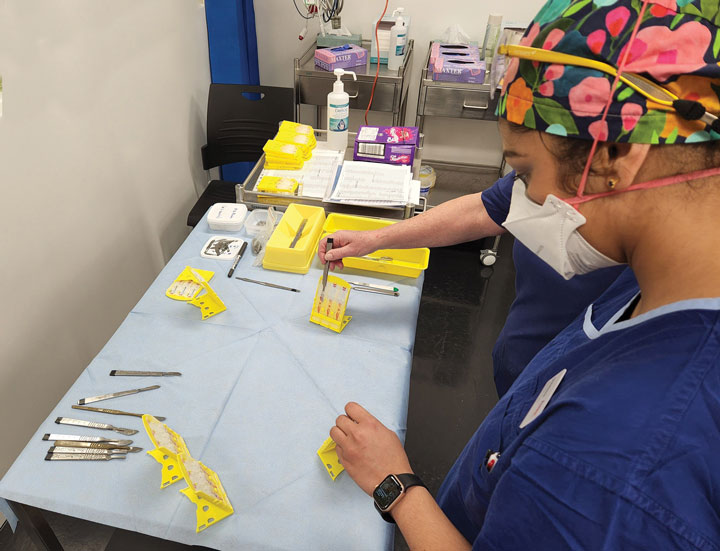
Pass it on
To prevent injuries during surgical procedures, the expectation should be set that staff will use hands-free passing to move blades, needles and other sharps through a neutral zone — the designated area for passing items from one staff member to another with the aid of a tray, magnetic pad or basin that eliminates hand-to-hand transfer. The location of the neutral zone should be announced during the pre-op time out. Surgeons, techs and nurses must clearly announce when sharps are placed in the neutral zone and keep their hands clear of the area until the items are removed by the intended recipient.
While neutral zone passing is a standard practice for surgical facilities of all kinds, OR teams can tailor this practice to bolster safety efforts.
“Wound closure is a particularly vulnerable time due to the many competing priorities that occur.”
Barbara L. DiTullio, DNP, RN, MA, CNOR, NEA-BC
For instance, Kaiser Permanente Panorama City (Calif.) Medical Center has two types — a pink transport tray for safe passing of any sharps in use and a non-traveling orange landing strip for sharps. The two areas assist during transfer and storage, both heightened times when staff are at greater risk.
“It’s understood as a designated area where contaminated and sharp surgical instruments are safely placed during a surgical procedure,” says Jennifer Yorke, MBA-HCM, BSN, RN, director of nursing for perioperative services at Kaiser Permanente Panorama City Medical Center. “The neutral zone is crucial for maintaining a safe and sterile environment, and it helps mitigate the risk of sharps injuries to the team.”
Even with right process in place, preventing sharps injuries requires a team that can minimize their distractions and maximize their focus. They must be aware of where sharps are at all times. It’s something that sounds simple and straightforward in theory but can be anything but in an action-packed OR.
“It’s critical for staff to keep their attention on what they’re doing while they are doing it,” says Dr. DiTullio. Multitasking, of course, runs contrary to this task-at-hand philosophy, and it’s a common problem area that facilities should watch for. “We tend to think we are quite skilled at multitasking, but at a time when there may be haste to ‘finish,’ engaging in multitasking creates difficulty in one’s ability to prioritize which is ‘most important,’ and leaves a gap where injury can occur,” she says.
Effective leaders find a variety of ways to drive home the importance of single-mindedness and hyperfocus, using a range of examples. Dr. DiTullio likens this intense concentration on the here-and-now to the martial arts term Mushin. “It translates to ‘no mind’ and describes a state of calm, focus, clarity and lack of mental clutter,” she says. “Conceptually, this means not looking forward to what is next, nor backward to rethink a comment or action that has passed.”
Safety is personal
Because providers focus so much of their efforts on their patients, their own protection sometimes gets short shrift. Sharps safety requires leaders to continually check in with their teams to make sure the culture is where it should be. “It’s so important for staff to raise awareness to foster a culture where staff prioritize their own personal safety,” says Dr. DiTullio. “Caregivers must care for themselves to properly care for others.” That, she adds, means putting incidents under the microscope and regularly reviewing injury reports to better understand the context in which injuries occurred and the activity that was happening at the time.
“Review injury reports on a regular basis and do the comparative work necessary to identify problematic trends that these reports reveal,” says Dr. DiTullio. “Make this information visible to staff so the importance of preventing injuries and keeping themselves safe is top-of-mind.” OSM
Every facility with a strong culture of safety relies on sound policies and clear communication to guide its daily operations. Of course, effective policies require regular review, updates and staff training. When it comes to sharps safety, Barbara L. DiTullio, DNP, RN, MA, CNOR, NEA-BC, senior clinical director of perioperative safety, quality and compliance at Beth Israel Deaconess Medical Center in Boston, advises facilities to keep the following elements front and center:
• Preach safe handling. One of the best ways to prevent sharps injuries is to spell out exactly how these instruments must be handled. Dr. DiTullio says facilities should emphasize hands-free handling of sharps to prevent direct contact and reduce the risk of injury when these instruments are passed from one team member to the next. Needles, she adds, should not be loaded or removed with another instrument.
• Think beyond the OR. Sharps injuries don’t only occur in the OR. Dr. DiTullio says sharps safety policies and procedures should extend beyond this space to keep everyone in the facility safe. Specifically, sharps should be separated from other instruments before sending them to sterile processing departments. “There have been a few times where I’ve seen a dermatome (blade from a skin mesher) make its way from the OR through SPD/CPD and back to the OR without anyone being injured,” she says. “Besides being unsterile, we were extremely fortunate no one was injured in handling this razor-sharp blade throughout the decontam process all the way back to the OR!” Because SPD staff are responsible for decontaminating, cleaning and ensuring sterility of all instrumentation, they are also vulnerable and should not be overlooked in sharps safety efforts.
• Use aids strategically. Safety scalpels, blunt-tip suture needles that can eliminate the chance of needlesticks thanks to non-bevelled tips, and plenty of other devices on the market can be wonderful resources to buoy surgical facilities’ sharps safety efforts, but each requires careful consideration among decision makers. “While safety devices have had a tremendous impact in reducing needle injuries overall, many of the devices designed to reduce injury do not lend themselves to the operative environment,” says Dr. DiTullio. For instance, she says, blunt-tip suture needles should be used when possible, but should not interfere with tactile functioning. Do your homework, trial the products and be sure the safety devices you are considering will work in real-life situations for your team.
• Double-glove for twice the protection. In addition to adding an extra layer of safety, this tactic can reduce exposure to bloodborne infections. “Indicator gloves are also a tremendous help in recognizing the outer glove has been perforated,” adds Dr. DiTullio.
• Prepare for the worst. OR teams need to know exactly what to do in the event of a sharps incident. “Most importantly, there must be a clear, well-articulated policy on how to get an injured staff member to occupational health ASAP following an injury and a patient-testing process that can be facilitated quickly and smoothly,” says Dr. DiTullio.
—Jared Bilski
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)