- Home
- The Magazine
- Article
Workforce Pulse: 2024 Salary Survey
By: Joe Paone | Senior Editor
Published: 1/25/2024
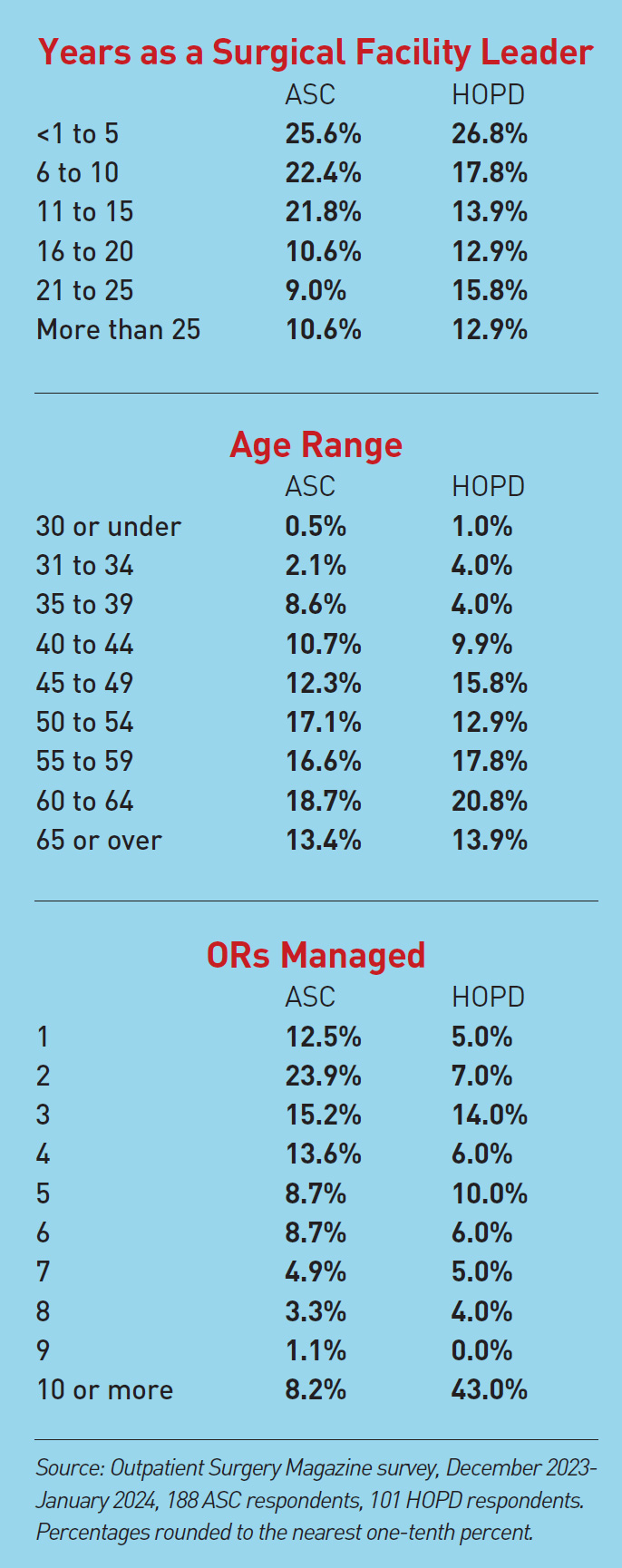
Outpatient Surgery Magazine’s annual analysis of our readers’ compensation packages also dives beneath the data to take leaders’ temperatures on a variety of issues.
Last year was another grind for leaders of outpatient surgery centers. Staffing concerns created a white-knuckle ride at many facilities that found it difficult to retain and recruit clinical and operational staff in the face of the larger salaries and superior benefits offered by large hospital systems and travel nursing opportunities.
Reimbursement and regulatory issues muddied the financial waters for some centers. Demand for services and surgical volume continued to grow, but so did competition, much of it better-funded than many freestanding facilities.
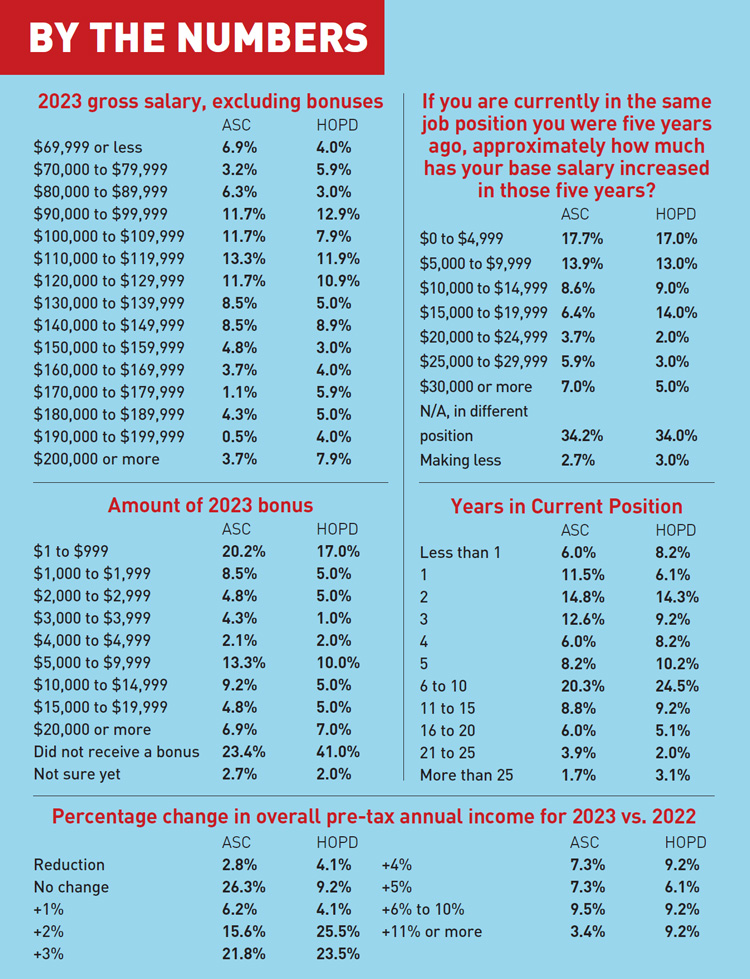
Salaries, bonuses and benefits
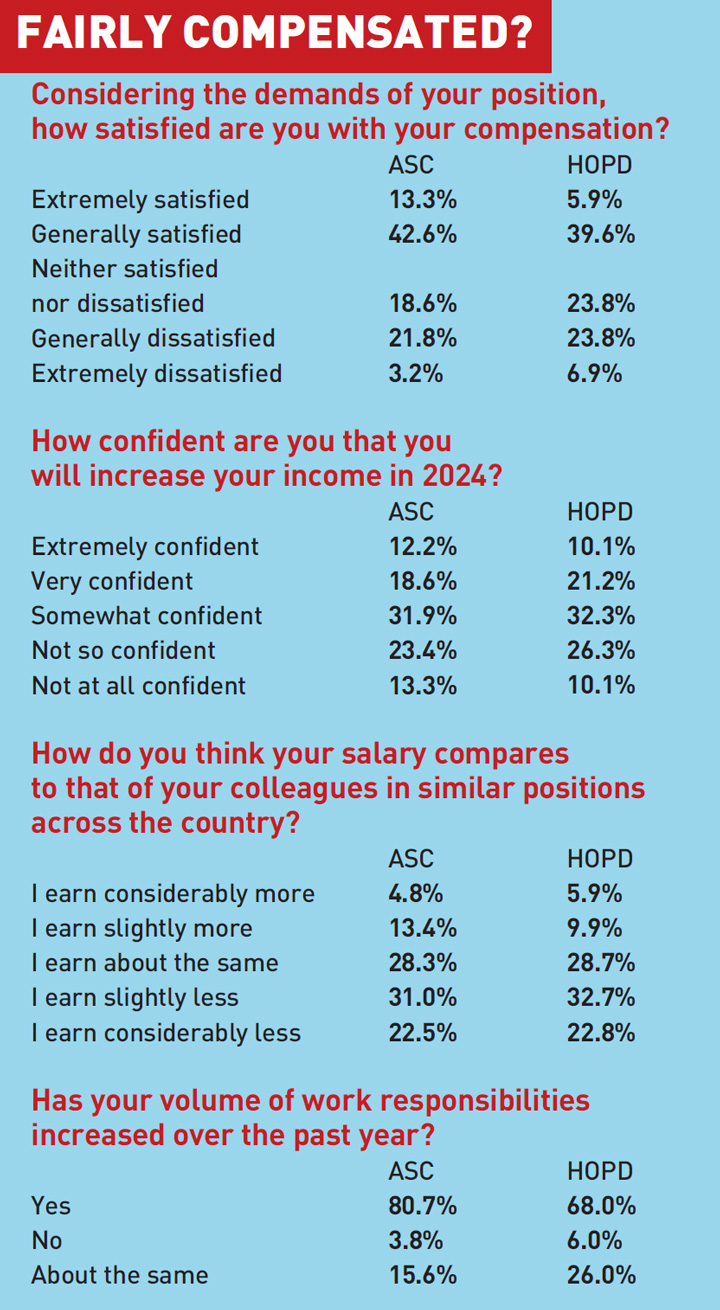
In terms of their own personal compensation, most respondents to the 2024 Outpatient Surgery Magazine Salary Survey remained relatively satisfied with their salaries, bonuses and benefits. But more than half of these outpatient surgery leaders also reported that they don’t believe they are making as much as their colleagues across the country, and expressed a lack of confidence that they will increase their income in 2024.
Meanwhile, a sizable majority reported that their volume of work responsibilities increased over the past year.
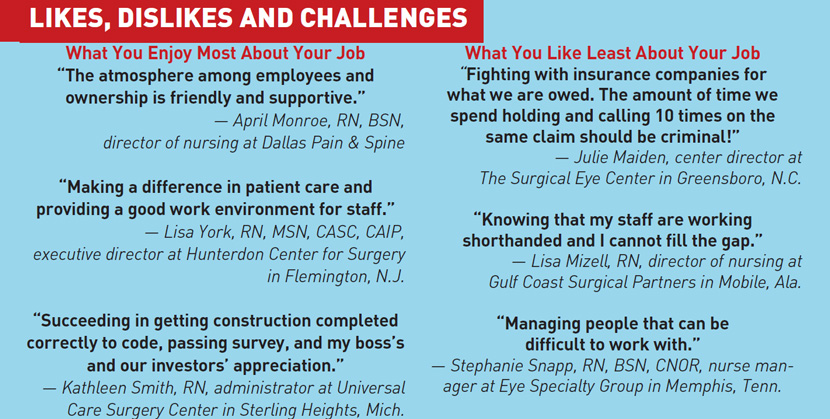
“I’m definitely not paid enough,” says Norma Bacon, administrator at New England Surgery Center in Beverly, Mass., who says she works nights and weekends to make sure everything gets done. “I do it all — HR, AR/AP, contract negotiations and currently managing an expansion.” Melissa Parsons, RVT, surgical director at Premier Vascular Center of Maryland in Towson, offers a similar “wearing too many hats” report. “I feel like I could be paid more,” she says. “I manage every aspect of my facility —accreditation, invoices, HR, etc.”
Tiffany Courington, RN, nurse manager at Laser & Cataract Surgery Center of South Georgia in Valdosta, feels her compensation doesn’t align with her responsibilities. “I continue to lead my team, I am always improving our efficiency and our volume continues to increase,” she says. “[But] if you look at the data, I am still paid lower than the mean for my position.” Tricia Huffman, surgery manager at PSI Surgery Center in Centerville, Ohio, likewise believes her compensation doesn’t align with the broader market. “I wear many hats and have seen what the average pay is in our area for my position,” she says.
On the mark
Still, many other respondents, like Nikki Zwick, RN, BSN, director at ENT The Surgery Center in Fort Wayne, Ind., believe their compensation does align with their responsibilities. “I also receive a nice bonus for the extra work that I do,” she says. Like many in the industry, she enjoys the more structured nature of outpatient surgery. “I have a good work-life balance since we are an ASC with no weekends, holidays or call,” she says.
‘No, really, how are you doing?’
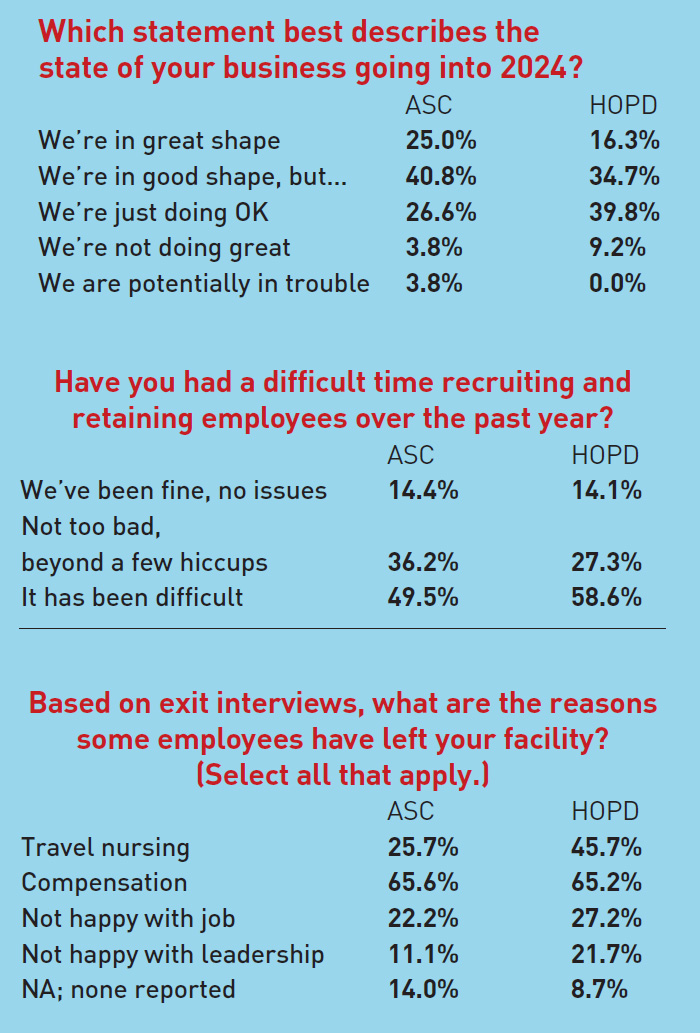
This year, for the first time in the history of our survey, we asked respondents about the state of their businesses. The general consensus was that most outpatient surgical facilities are doing fine, but many feel they possess the potential and the initiative to do even better. However, market forces such as regulation, reimbursement, staffing and competition were reported as significant hurdles for many centers.
April Monroe, RN, BSN, director of nursing at Dallas Pain & Spine, gave a representative response, described her practice as “just doing OK.” “The last year was financially less productive than years past and we saw a loss for 2023,” she says. “However, measures have been taken to identify the areas where loss of revenue occurred and corrective action has been initiated that project a significant improvement for 2024.”
Karely Deal, center director at Centinela Valley Endoscopy Center in Inglewood, Calif., touches on a common existential feeling: “We’re in great shape at the moment because we have enough staff.”
“Every single work responsibility has substantially increased,” says Michelle Morrison, RN, BSN, director at Eye Surgery Center of Wooster (Ohio). “Our patient volume is higher than ever before but we are functioning with about the same number of employees.”
Debbie Cooner, administrator/CEO at Outpatient Services East Surgery Center in Birmingham, Ala., evokes the constant concern about staffing as well as another recurring concern in the industry. “We are in really good shape but something like a huge anesthesia stipend or staffing shortage could change that quickly,” she says.

Course correction
An intriguing course correction regarding the volatile anesthesia services situation is under consideration at Eltra Surgery Center in Florham Park, N.J. While reporting the center is in great shape, Clinical Director Jeaneen Dwyer, MSN, notes that “the only obstacle I foresee is lack of anesthesia services, which is why we are evaluating more procedures performed under local anesthesia.”
Lara Kirchner, RN, MSN, clinical director at Fairfax (Va.) Surgical Center, selected “We’re in good shape, but...” She says volume not only remains steady but even is increasing from pre-pandemic levels, while noting that capital purchases the ASC made in 2023 have improved staff and especially surgeon morale. “We are no longer hearing, ‘Well, such and such hospital has them, why don’t you?’ from our surgeons so much,” she says. Mark Spina, MS, director of operations at Endoscopy Center of Connecticut in Hamden, reports that his practice is in “good shape” financially, but adds that “rising labor costs and lack of increases in payor contracts will constrict margins.”
Staffing is still a huge problem
Outpatient facilities once again reported staffing issues as one of their most consistent concerns, with roughly half characterizing the situation as “difficult,” and just one out of every seven centers reporting zero staffing issues. The dominant reason was compensation.
Julie Maiden, center director at The Surgical Eye Center in Greensboro, N.C., reports that recruiting and retention has been difficult. “Traveling nurse salaries have made it nearly impossible for small centers to get good and experienced staff,” she says.
Can’t compete for comp
Eye Center of Columbus (Ohio) reports its staffing situation has been “not too bad,” but market changes carry the potential for it to deteriorate. “Columbus has built several new hospitals and we cannot compete with their compensation,” says Administrator Mary Meier.
“The nursing community is moderate-size for the area we live in, but we are unable to compete with the two major hospitals and their benefit packages,” says Erin Foley, RN, BSN, clinical manager at Baptist Beaumont (Texas) Surgical Affiliates. “There are not enough nurses that want to work for a smaller company with a less of a package.”
Tri-City Surgery Center in Prescott, Ariz., reports tough sledding. “We struggled as we cannot compete with hospital pay rates,” says Karla Perry, BSN, RN, nurse administrator and director of nursing. “Also, travel nursing has made it almost impossible for us to compete to those salaries.”
Debbie Cooner, administrator/CEO at Outpatient Services East Surgery Center in Birmingham, Ala., says her staffing situation wasn’t too bad in 2023, but sees worrying signs ahead. “We live in a city that has multiple medical centers and ASCs,” she says. “The staffing shortages have resulted in a wage war that makes it difficult to keep staff without a larger-than-normal ASC salary. At some point, it will be difficult to sustain if this does not slow down.”
The labor pool is underwhelming many centers. “The quality of staff we are interviewing has decreased,” says Beverly Ann Kirchner, MSN, compliance officer and clinical resource director at Trias MD in Highland Village, Calif. “We struggle finding experienced OR staff, scrubs and circulators,” says Lisa Mizell, RN, director of nursing at Gulf Coast Surgical Partners in Mobile, Ala. “My current staff are worn out due to a staffing shortage. We have lost good employees because of the late working days.” Norma Bacon, administrator at New England Surgery Center in Beverly, Mass., calls front desk help “nonexistent.”
“I am amazed with the number of applicants who have ghosted on their interviews. It has been very frustrating,” says Lara Kirchner, RN, MSN, clinical director at Fairfax (Va.) Surgical Center, who nevertheless reports recent improvements. “Staffing has improved exponentially in the last few months of the year and I am hopeful that 2024 will see significantly less turnover and overall improved morale and performance for staff and the center as a whole.”
Coming soon
We asked respondents about new initiatives, programs or additions their facilities are planning for 2024. We also asked about the opportunities and threats your facility sees over the coming year.
It was an illuminating exercise in many regards, and responses painted a telling picture of what surgical leaders are excited about — as well as what they fear.
One typical response was from Erin Foley, RN, BSN, clinical manager at Baptist Beaumont (Texas) Surgical Affiliates. She says the biggest opportunity her practice sees for 2024 is establishing new service lines. The biggest threat? “Not being able to staff the new service lines,” she says.
Leaders at many centers expect to expand their service lines or facilities this year. Dallas Pain & Spine intends to expand and open a secondary facility, while ENT The Surgery Center in Fort Wayne, Ind., is building a new facility to accommodate its growing practice. Casper (Wyo.) Surgical Center plans to expand along with purchasing new capital equipment and possibly starting a robotics program. VHC Health in Arlington, Va., is renovating to accommodate new service lines and equipment, while Heartland Surgery Center in Kearney, Neb., is growing its spine, ENT and urology service lines by adding new procedures and equipment that were purchased. Texarkana (Texas) Surgery Center is adding cardiology and corneal procedures.
Threats to watch
Many leaders described the diverse threats they see coming this year. Those include increased payroll and other costs, decreases in reimbursements for certain procedures (and the difficulty of balancing expenses against those reimbursements), backordered supplies and medications, inflation and the economy (especially for facilities that are private-pay only), the possibility of being purchased by a larger company, and maintaining adequate staffing levels for all provider types, including nurses, techs and anesthesia providers.
Other respondents had less concrete and more existential concerns about what lies ahead to potentially disrupt or even destroy their business prospects in the future. For example, when asked about the threats he sees affecting his facility, Stephen Gatesman, RN, BSN, clinical director at Executive Park Surgery Center in Fort Smith, Ark., simply replied, “Being stagnant.” OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)