Efforts to achieve positive outcomes begin as soon as procedures are scheduled.
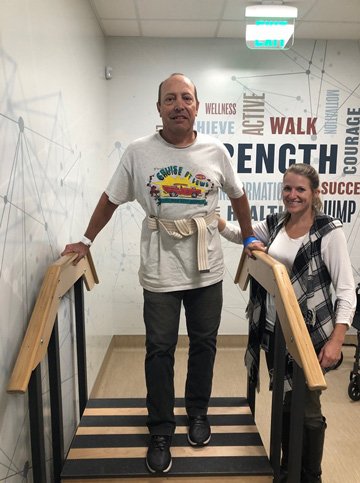 STEPPING UP Patients who are physically active before joint replacement surgery are better prepared to complete post-op rehab programs.
STEPPING UP Patients who are physically active before joint replacement surgery are better prepared to complete post-op rehab programs.
Increasing numbers of total joint replacements will be performed in outpatient facilities as long as providers prioritize reducing negative outcomes that lead to unplanned readmissions. That requires optimizing perioperative care, addressing complication risk factors and clear communication with patients, according to a new paper.
Several criteria should exclude patients from undergoing elective joint replacements in the outpatient setting, according to the paper published in the Canadian Medical Association Journal: pre-op bleeding disorders, liver cirrhosis, renal disease of stage 2 or greater and an inability to participate in pre-op education. The authors also note patient-specific factors that should give providers pause before proceeding with joint replacement surgery: age 80 years or older; ASA classification greater than two; severe obstructive sleep apnea; history of cardiac disease; diabetes; body mass index greater than 35; and a lack of a social support system at home.
The authors add that post-discharge surveillance through follow-up phone calls or technology that provides remote real-time monitoring of a patient’s condition, as well as regular wound checks for infection, are essential to achieving positive outcomes after joint replacement surgery. Addressing modifiable risk factors can also reduce complications and readmissions. For example, they say having smokers kick the habit and optimizing patients' nutrition status leading up to their surgeries can prevent adverse events and reduce the risk of unplanned hospitalizations.
Surgeons and primary care physicians play important roles in setting the right mindset in patients for same-day surgical success. The paper's authors point out that even some patients who believe they can recover safely and comfortably at home enter surgery expecting to be hospitalized for at least a couple days. Communicating clearly with patients, beginning at the time of referral for surgery, about expected levels of pain and the recovery process can set realistic perceptions about the feasibility of same-day discharge and the active role they play in achieving positive outcomes.
"Protocols continue to evolve," say the authors. "However, patient safety must remain the priority with any change. Careful education of patients can help shift misconceptions about outpatient total joint procedures and optimize success."
.svg?sfvrsn=be606e78_3)



.svg?sfvrsn=56b2f850_5)