The choice between posterior and direct anterior approaches, both effective and safe, boils down to surgeon preference.
 CREDIT: Patrick Toy
CREDIT: Patrick ToyWHICHEVER WORKS Surgeons are split on their preferred approach to knee replacements, but fortunately both primary options are clinically effective.
What's the best surgical approach to replace hips: posterior or direct anterior? Both techniques come with inherent advantages and disadvantages, but the literature and anecdotal debate largely find basic agreement that both approaches are safe and effective — it’s really all about what the surgeon feels most comfortable doing.
Posterior approach. With this method, the incision is made on the side of the hip, above the greater trochanter of the femur, and the dissection goes behind the abductor muscles. Daniel Pincus, BA&Sc, MD, PhD, FRCSC, a joint replacement specialist and an assistant professor at the University of Toronto Sunnybrook Holland Orthopaedic Centre, says patients operated on with this approach usually recover with no risk for long-term abductor dysfunction or chronic limping. "The posterior approach is also the most extensile, making it the primary option for revision surgery," he says.
Joshua C. Rozell, MD, a hip and knee reconstruction specialist at NYU Langone Orthopedic Center in New York City and NYU Langone Ambulatory Care Bay Ridge in Queens, says the posterior approach is generally easier to perform because the hip is more accessible from the back than from the front. "Surgeons achieve easy extensibility of the incision and greater exposure for better access to the implant's femoral stems," he says.
Other advantages of the posterior approach include less blood loss, faster surgical times, less anesthesia prep time, and the fact that fluoroscopy and a specialized hip table are not required, says R. Michael Meneghini, MD, director of the Indiana University Health Hip and Knee Center and professor of clinical orthopedic surgery at Indiana University School of Medicine in Indianapolis. He believes this gives the approach a leg up in surgery centers.
Disadvantages include higher rates of post-op joint instability and slower recoveries than the anterior approach. Concerns about intraoperative dislocations have eased, but improved surgical technique and implants with large diameter bearing surfaces have lowered rates to levels on par with the anterior approach, says Dr. Pincus.
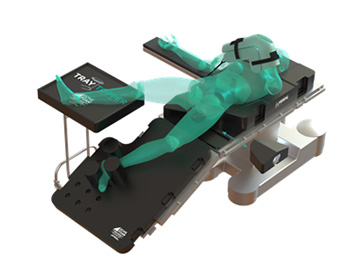
Direct anterior approach. With this technique, surgeons enter the joint through the internervous plane and between the abductor muscles, leaving external rotators and tendons intact. Dr. Pincus says this muscle-sparing approach facilitates faster early recovery in theory, but more data is needed to confirm this. Dr. Rozell says this approach allows surgeons to better measure leg length, which he says is more difficult to do with the posterior approach. He believes the anterior approach is cleaner and that its preservation of soft tissue makes it more conducive to outpatient procedures. "Anecdotally," he adds, "I've found joint stability is typically better than with the posterior approach."
Dr. Meneghini says disadvantages associated with the anterior approach include increased risks of femoral fracture, nerve injuries, infection, femoral component loosening, anterior groin pain, iliopsoas impingement and wound complications. Another disadvantage involves the location of the incision near the groin. "The skin and underlying tissue and fascia are less robust for closure compared with the side of the hip where the posterior approach is performed, which has led to an increased risk of wound breakdown and prosthetic joint infection," he says.
Dr. Pincus says the direct anterior approach limits the femoral access needed for inserting the implant's stem, but surgical techniques and technology are addressing this limitation.
Approaches to the hip are typically based on the preferences of surgeons, who often use the one they're most comfortable performing or the one they were taught during residency. “The way surgeons are trained plays a big role in the approach they choose,” says Dr. Rozell. Adds Dr. Pincus, "Despite all our work on this topic, I still believe the choice of surgeon is much more important than the choice of approach."
.svg?sfvrsn=be606e78_3)


.svg?sfvrsn=56b2f850_5)