- Home
- Article
Building a State-of-the-Art Total Joints Program
By: Kendal Kloiber | Contributing Editor
Published: 11/21/2023
Here’s a blueprint to get your outpatient arthroplasty program up and moving.
A top-notch total joints program represents the pinnacle of innovative practices, where cutting-edge technology, strategic staffing and meticulous patient selection converge to create an unparalleled healthcare experience.
“We’re witnessing a transformative shift toward exceptional care at lower costs in surgery centers, ensuring a sustainable and financially responsible approach,” says Phillip Bostian, MD, orthopedic surgeon at EmergeOrtho in Newtown, N.C. “Our commitment is clear: to provide excellent care without cutting any corners, offering patients the best possible joint replacement experience.”
Expert insights
Here are the top tips and insights from experts for setting standards that define these programs and keep their facilities consistently in high demand.
When it comes to setting the stage for a successful total joints program, patient selection is at the heart of it all, says Dr. Bostian. He says there are several key things he looks for in his patients to make sure they’re the right fit for the ASC environment, the first being that they don’t have uncontrolled sleep apnea. If he suspects sleep apnea in a patient based on a thick neck size or self-reported bad snoring and they don’t actively use a CPAP machine, then that patient is automatically excluded from consideration for same-day discharge.
Other comorbidities he looks for include patients who are on pain medications preoperatively — due to the higher likelihood they will have uncontrolled pain after surgery — and those who have active organ failure. Patients who are morbidly obese often have their surgery done at the hospital as well, though they may still be discharged the same day depending on how they progress.
“Some patients simply aren’t appropriate to be done in a surgery center from a health perspective,” says Dr. Bostian. “We are very judicious about our patients. If there’s a patient we’re on the fence about, we do it at the hospital so we can admit them if necessary.”
As the population in its area experiences a significant influx, St. Luke’s Health System in Idaho recognizes the importance of caring for patients beyond the surgical suite. A fundamental aspect of its program involves implementing and establishing a proactive strategy that begins well before patients even sign up for surgery, says Tim Nicolello, orthopedic service line manager.
St. Luke’s takes a holistic view, pairing patients with providers to address health indicators such as BMI, pain medicine usage, A1C levels and mental health status. These risk factors play a pivotal role in influencing the outcomes of joint replacement surgeries, says Ronald Kristensen, MD, director of joint replacement at St. Luke’s. By focusing on improving these factors before surgery, St. Luke’s aims to not only improve surgical outcomes but also enhance the overall well-being of its patients.
Managing patient expectations
Another key feature to success is letting the patient know what to expect before their total joint replacement. Dr. Bostian notes that one of the most important parts of this is determining what support the patient has at home. He and his staff work extra closely with patients who live alone, including talking to their families to make sure they will have the support they need when they’ll be home several hours after their procedure.
“It’s mandatory that they have help at home for the first week,” says Dr. Bostian. “Sometimes they worry about bothering their family members, but I try to stress to our patients that they likely do have someone who is more than willing to take care of them. They just need to ask.”
In addition to setting the groundwork for the support needed post-procedure, Dr. Bostian and his team work with patients to “give them a sense of what things will be like when they get home.” That means setting reasonable expectations about things such as bruising, pain and movement to make sure patients know what hurdles to expect on the road to recovery.
“We try to address what the most common complaints are after surgery,” he says. “We make sure they have the prescriptions for anti-nausea medicine and pain medicine at their fingertips, so that they have everything they need. That ultimately cuts down on phone calls and trips to the ER.”
His facility also relies on technology to help with this process. The center is piloting an app that helps to communicate with patients, allowing them to review videos about the procedure, information on exercises to do while recovering, as well as the ability to message with their care team. It also collects outcome measurements as they recover.
“We can go in and see who’s doing well, and who’s struggling, which means we can bring them in sooner if we need to and get them the help they need,” says Dr. Bostian.
Embracing technological marvels
New technologies are also promising to make outpatient total joints easier and more efficient for facilities. Zachary Yenna, MD, hip and knee replacement surgeon at St. Luke’s, notes that the use of robotics, while not proven to provide better outcomes, does make things more precise and customized for the patient. He says that the robot allows the surgeon to make cuts on the bone that work perfectly with the patient’s anatomy, providing a surgery that’s more individualized than standard procedures.
“Traditionally, you made a cut based on what the surgeon believed to be true,” says Dr. Yenna. “So, you could say you want to remove 8mm of bone, but with the nature of old jigs and based on the precision of your eye, you could actually be removing 7 or 10 mm. Now, with the robot, if I want to take off 10.5mm of bone, we do.”
Other innovations such as navigation systems offer real-time insights into joint alignment and movement. “Navigation systems can definitely help to improve efficiency,” says Dr. Bostian. “I think they can minimize outliers and may potentially improve outcomes.” However, he notes that the important thing to him when it comes to technology is that it’s offered to patients consistently—whether they’re getting their joint replacement at the hospital or the ASC.
“Some surgeons feel that a robot enhances their ability to deliver a high-quality joint replacement, and if that’s the case, then they should use it,” says Dr. Bostian. “Others don’t feel it’s necessary. Technology should be a question of giving the best joint replacement to the patient.
“I tell my patients that regardless of where I take you, you are getting the Cadillac of joint replacements,” he adds. “If I use a robot at the hospital, then I use a robot at the surgery center. I don’t think we should change things simply because we’re at the surgery center and trying to be more lean and more efficient.”
Supreme staffing
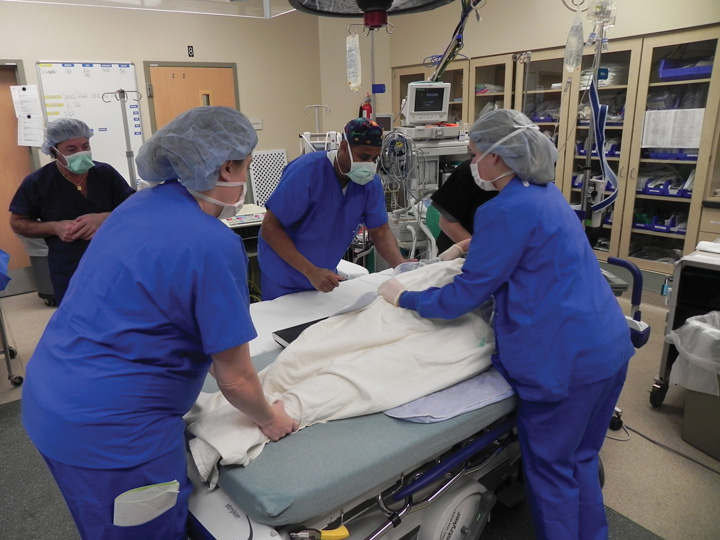
In the realm of state-of-the-art programs, the heartbeat of excellence is a dedicated and synchronized team. The emphasis on staffing is not merely a logistical consideration but a fundamental component that shapes the success and efficiency of outpatient total joints.
Mr. Nicolello notes that regular meetings with providers create a friendly space for sharing insights and bringing everyone together to understand each step of patient care. In these collaborative chats, it’s not just about what works, but why it works. He explains how they tackle differences in practices between sites, breaking down everything from pre-op routines to post-surgery care. A recent meeting included a deep dive into the details of anesthesia, looking at pain management and how to get patients moving after surgery. The goal? Not just to smooth out the bumps but to raise the bar for care in all six centers.
“We all meet frequently to talk about things that work and don’t work at a systemwide level,” adds Dr. Yenna of his colleagues at St. Luke’s. “We talk quite a bit, which helps us correct any issues that may arise.”
Dr. Bostian notes the pivotal role of having a consistent and dedicated OR team. This team comprises the same staff members for every surgery, creating an environment where familiarity breeds unparalleled efficiency. The dedicated teams are well-versed in each surgeon’s preferences, ensuring a standardized approach to every surgery. He highlights that by having the same surgical technologist on every case, there is a seamless exchange of instruments that transcends verbal communication. The goal is clear: to perform joint replacements without the need for unnecessary communication, promoting an efficient workflow.
“My surgical technician knows every step inside and out,” says Dr. Bostian. “It’s very important to have it that way because it makes it so much faster.”
Dr. Bostian credits his facility’s efficiency to having two dedicated OR teams. As one patient’s surgery concludes, the team seamlessly transitions to the next case, turning over responsibilities in the most efficient way possible. The absence of downtime is a testament to the efficiency and expertise of the staff involved, he says.
Additionally, the importance of having all instruments readily available cannot be overstated. Dr. Bostian introduces a strategic approach, with several instruments peel-packed and ready to go on a shelf in the OR. This ensures that in the event of any unforeseen circumstances, such as a dropped instrument, the team can swiftly adapt without disrupting the flow of the surgery.
“Everybody knows their job, and they do it very well,” he says. “Staff matter. When you have people who are courteous and kind, that impacts the overall patient experience.” OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)