We recently asked several forward-thinking ENT surgeons for insights on innovations that improve outcomes and enhance patient care. Removing the thyroid from inside the lower lip, maneuvering instruments along pre-planned virtual pathways during sinus surgery and freezing nerves to solve chronic sniffling were among the buzz-worthy developments that have them excited about their specialty’s future.
- Home
- The Magazine
- Article
New Opportunities in ENT
By: Joe Paone
Published: 11/14/2019
Get up to speed on hot trends in thyroid, sinus and sleep apnea surgeries.
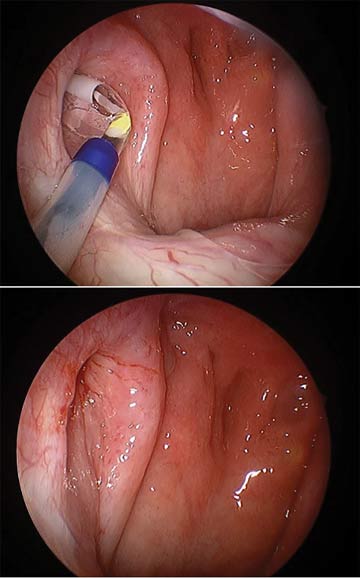
1. Transoral thyroidectomy
This “scarless” laparoscopic procedure lets surgeons remove the thyroid via a vestibular approach instead of open surgery. Jonathon Russell, MD, director of endoscopic and robotic thyroid and parathyroid surgery, and assistant professor of otolaryngology, at Johns Hopkins Medicine in Baltimore, Md., is one of the surgery’s pioneers. He says surgeons make a 1.5-cm incision in the gingival sulcus and 2 stab incisions at the oral commissure. They then tunnel down through the incisions, dissect around the thyroid and remove the gland through the central incision.
“It’s a great approach, because it doesn’t require any additional instrumentation, and it doesn’t take too much extra time over the traditional surgery” — about 15 additional minutes, says Dr. Russell. “And patients can still go home same-day. In every way, it’s the same surgery except for no scarring.”
Transoral thyroidectomy, however, can be a somewhat radical adjustment in terms of technique for surgeons. “It’s a different skill set for most thyroid surgeons who are accustomed to using open instrumentation,” says Dr. Russell. “It lends itself well to surgeons who have laparoscopic skills.”
The learning curve is short — about 10 cases — but high-volume thyroid surgeons are often booked 2 months in advance, so it’s difficult for them to take on these cases to master this technique. That’s been the biggest hurdle to widespread adoption, according to Dr. Russell, who champions making the technique more widely available. “It’s better for patients,” says Dr. Russell.
“Certainly, we’ve seen very happy patients [who have the procedure done].”
2. Ablation of thyroid nodules
Guided by ultrasound, the surgeon inserts a radiofrequency probe that heats up the nodules, which activates the immune system and, over time, causes scarring and shrinkage of the nodules. The procedure takes half an hour or less. “[Recovery] is clearly not as quick as it is with surgery over the long term, because you have to wait for the immune system to come in and cause the scarring and clean up the dead cells,” explains Dr. Russell. “But over the course of a year, you can see 80% to 90% shrinkage in the nodule, and almost all patients have a significant improvement in their symptoms.”
Dr. Russell says about 80% of Americans have a thyroid condition and notes this procedure could prove “revolutionary” for same-day surgery centers in terms of how they treat thyroid pathology.
“It’s a really exciting technology,” he says. “I think it’s going to be used for a fair percentage of the thyroid nodules business in the very near future.”
3. Implants for nasal valve collapse
Traditionally, correcting valve collapse involved rhinoplasty. With this option, the surgeon simply makes a stab incision, passes an instrument into the correct area and deploys the implant. “It creates a scar or an inflammatory reaction, with the goal of stiffening that area to prevent collapse,” says R. Peter Manes, MD, FACS, an associate professor of otolaryngology at Yale School of Medicine in New Haven, Conn.
The procedure is said to lead to quicker recoveries and shorter surgical times than the traditional surgery for this condition, during which grafts must be harvested and additional incisions made.
4. Cryotherapy for rhinitis
Patients with perpetually runny noses often run out of patience when looking for a cure. “We don’t have a lot of good treatment options for them,” says Dr. Manes. “We can give them nasal sprays, which sometimes work and sometimes don’t.”
Enter cryotherapy, something of an older technology that’s been modified for use in the nose. Surgeons apply cryotherapy to the posterior nasal nerves, which often provide the stimulus that causes constant nasal drip, and freeze them. Dr. Manes says the procedure can be done “fairly quickly” in an OR or even an office setting with minimal instrumentation. He also says the procedure is “very well tolerated,” with the main complaint from patients being that they get something of an ice cream headache.
5. Sleep apnea innovations
New surgical techniques are emerging for the growing problem of sleep apnea. Robson Capasso, MD, chief of sleep surgery at Stanford Health Care in Redwood City, Calif., says hypoglossal nerve stimulation (HGNS) involves implanting and activating a pacemaker-like device in the patient. Unlike soft tissue and skeletal surgery treatments, both of which cannot be reversed, the implant can easily be removed.
The risks of HGNS, says Dr. Capasso, are small. It leaves 3 scars — one below the right side of the jaw, one in the chest and one on the right side of the ribcage. Most patients feel a mild degree of discomfort in the tongue. And like any implant, it carries a small risk of infection. But recoveries are much less lengthy and painful with the implant compared with the other surgical techniques, says Dr. Capasso.
6. Dilation of the eustachian tube
This procedure, which equalizes air pressure for patients who suffer from the common condition of eustachian tube dysfunction, uses technology similar to that used for balloon dilation of the sinuses. “You place this balloon in the eustachian tube under visualization, and you inflate that area,” says Dr. Manes. “You’re creating a better opening to allow equalization of pressure.” He says some surgeons have been performing this procedure for a while, but adoption is growing as more literature about it emerges.
7. Enhanced sinus surgery

Software that provides facial mapping, image guidance and pre-operative planning is emerging as a valuable tool during sinus surgery. “It’s an extra level of confirmation and certainty that you’re actually in the spaces you want to be,” says Brent Senior, MD, FACS, FARS, chief of rhinology, allergy, and endoscopic skull base surgery, otolaryngology/head and neck surgery at University of North Carolina at Chapel Hill, and vice president for development and strategic initiatives with the American Rhinologic Society. He adds that the technology could be particularly useful for navigating around dangerous areas like the sphenoid sinus.
The system also provides the ability to preoperatively mark anatomical targets and anti-targets. “For example, you would mark the anterior ethmoidal artery, which is dangerous if it were injured during sinus surgery,” says Dr. Senior. “We mark that on the CT scan, and the system will make an auditory ping to let us know we’re getting close to that vessel.”
Dr. Senior uses the technology to see what he removed from the sinuses. “It keeps track of the movement of your suctions inside the sinuses during the case, and gives you a virtual picture of areas where the suction has traversed,” he says. “That gives you a good sense of all the areas you’ve operated in, and a general picture of the completeness of the surgery.”
Dr. Senior also touts facial recognition technology for the preoperative registration process, which prepares a 3D reconstruction of the face for the image guidance system to display during surgery. “All of the systems require that you register the patient’s CT image to the true anatomy of the patient,” he explains. For facial mapping, some systems run a laser over the face, while others require a physical touching of the face. Dr. Senior’s system uses a smartphone. “You can use your iPhone or iPad to take a picture of the patient’s face, and it registers in the system,” he says.
Surgeons can use image guidance software, the patient’s pre-op CT scan and facial mapping capabilities to virtually map out the surgery before they enter the OR. That plan is then visible through augmented reality technology during the procedure, letting surgeons follow the virtual path they created.
“The software allows you to study, for example, the patient’s frontal sinus, and really understand that anatomy,” he says.
“Then you can trace out the intricate pathway heading into the frontal sinus and the software overlays that pathway on a virtual image or even the real endoscopic images as you do the surgery.”
Does all of this technology provide the surgeon with a higher degree of accuracy, confidence and efficiency? “Without a doubt,” says Dr. Senior. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)