- Home
- Special Editions
- Article
Capitalize on the Outpatient Shoulder Boom
By: Adam Taylor | Managing Editor
Published: 8/26/2025
Early adopters of replacement surgeries at ASCs reveal the details that have made their programs successful.
Shoulder replacements have entered the outpatient realm in significant numbers and continue to grow, especially with Medicare reimbursements now a reality and robotic assistance on the immediate horizon. Surgeons who have been performing these relatively difficult procedures in ASCs and HOPDs even before regulations and technology widened the path have achieved stellar and reproducible results.
The way these procedures are being performed in ASCs is becoming more sophisticated and nuanced. For example, Brian Badman, MD, recently performed the first shoulder replacement surgery in Indiana that used a new augmented reality (AR) technology to increase surgical guidance without extra screens or additional bulky equipment.
High-tech headsets
Dr. Badman donned the AR headset for the procedure at an ASC in Fishers, Ind., on July 28, according to a blog entry on the Central Indiana Orthopedics website.
The technology Dr. Badman used allowed him to see surgical guidance directly through an eyepiece instead of looking away from the surgical site to view information on a screen across the room. Viewing the images he needed directly over the shoulder he worked on minimized the potential for distraction and allowed him to make highly accurate adjustments in real time.
“I’m able to make more informed and accurate decisions during shoulder replacement surgery,” says Dr. Badman. “It’s a smarter way to operate — one that keeps my attention where it matters most: on the patient.”
The AR system enables more personalized, precise surgeries because it helps surgeons more accurately align and position implants based on the patient’s individual anatomy. The hands-free and self-contained system allows surgeons to focus fully on the procedure and doesn’t require additional equipment in the room. This streamlined surgical environment make for more efficient procedures.
Robotic advances
In March, Ammar Anbari, MD, performed the first-ever robotic total shoulder replacement outside of a hospital anywhere in the world at Constitution Surgery Center East in Waterford, Conn. He says the robot will help shoulder surgeons who perform several total shoulder arthroplasties (TSAs) a week, but will be particularly useful for orthopods who do only several a year. Even for orthopedic generalists, robots produce error-free results, he says.
Rob Taylor, RN, BS, IP, CFDAI, the ASC’s clinical director and total joint coordinator, recommends facilities conduct a financial analysis to see if the robot’s seven-figure price tag makes sense.
“I’m able to make more informed and accurate decisions during shoulder replacement surgery.”
—Brian Badman, MD, on augmented reality
Robotics are making significant inroads in total joints procedures of all kinds at hospitals, HOPDs and ASCs. This will only continue as the units get smaller and the patient pool gets older — and will positively impact the outpatient shoulder market. A Mayo Clinic Arizona study, for example, says patient expectations will continue to rise after their research on 10 years of Google trends showed a significant jump in public interest in robotic total joint arthroplasty from 2011 to 2020. As a result, more surgeons have made robotics part of their arsenal than ever before. By 2030, two of every three total hip arthroplasties will be done robotically, as will one in two total knee arthroplasties, according to the results of a Cleveland Clinic study.
More growth to come
Outpatient total shoulder replacements were approved by the Centers for Medicare & Medicaid Services (CMS) in 2024, years after the agency gave total knees and hips the nods for patients in ASCs. More outpatient total knee and total hip arthroplasty still takes place than total shoulders, but it’s gaining ground. The 2019 American Academy of Shoulder & Elbow Registry (AAOS SER) shows that 71.3% of patients were discharged to their homes from 2015 to 2000, while the 2024 AAOS SER puts the number at 79.1% from 2015 to 2023.
The boom should continue, according to shoulder surgeons who have spoken with OSM about what has made their outpatient shoulder services lines successful. Here are some of the best nuggets those leaders have shared.
TSAs are perfect for ASCs
Surprisingly, shoulder arthroplasty is less painful for most patients than other shoulder surgeries such as rotator cuff repairs, says David M. Dare, MD, a surgeon with Raleigh (N.C.) Orthopaedic. “Combine that with the nerve block we use, and our patients will take no pain medication, or very little, afterward,” he says. “Patients are surprised by the delta between their pre-op and post-op pain levels.”
Shoulder procedures are easier for patients to put off, simply because it’s easier to get around with one bad arm than it is with one bad leg. The recovery for shoulder patients is easier, however, because hip and knee patients must walk on their new joints right away, while a shoulder patient simply puts on a sling and avoids putting immediate pressure on it.
Patient education is a key component of a successful shoulder program. “It’s helpful to take the time necessary to explain the process to patients. I tell them it’s completely safe and that they’ll have very little, if any, pain after surgery,” says Dr. Dare. “Then I explain that it’s safer for them to be in an outpatient setting than an inpatient setting because of the lower risk of infection and other reasons.”
Patients simply do better at home, says Dr. Dare. They sleep well at night because they’re where they are most comfortable and aren’t bothered by sick patients and awakened by nurses through the night.
Dr. Dare has performed outpatient shoulder replacements for more than a decade and says other surgeons shouldn’t be reluctant to do so. “If you are at an outpatient facility and are accustomed to doing rotator cuff repairs, you’re already performing surgeries that are significantly more painful for patients in the immediate postoperative period,” he says. “Many of my total shoulder patients, on the other hand, have no pain postoperatively.”
Patients are pleasantly stunned to find themselves in PACU for less than an hour and home on a recliner or in bed just hours after they arrived at the ASC for their procedure, says Dr. Dare, who calls that scenario “a complete paradigm shift” from earlier eras of shoulder replacements.
Be consistent and efficient
The total shoulder program at Excelsior Orthopaedics in Buffalo, N.Y., is successful because it is driven by protocols and is consistent as a result, says Kory B. Reed, MD. The alignment of protocols for the cases of all surgeons allows for at least six total joint replacements of all kinds per day at its facility.
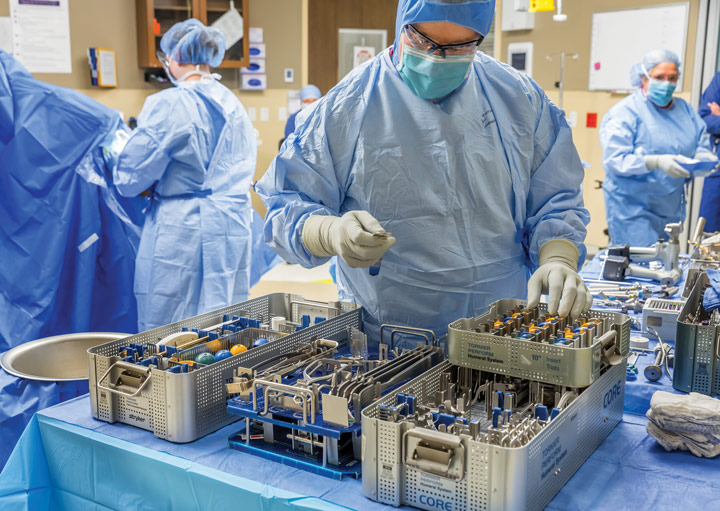
“We have consistent treatment protocols across the board, with only slight fluctuations form surgeon to surgeon,” says Dr. Reed. “Every surgeon wants what they want, but we’ve become very consistent in the implants we use, not all the same company, but we trimmed it down to companies that are best suited cost-wise, tray-wise and equipment-wise, so we’ve been able to reduce costs. We’ve also been able to streamline the processing of equipment to ensure sterility and accessibility of trays in the smaller-than-a-hospital surgery center environment. We’ve all made little compromises even for postoperative physical therapy, follow-ups and discharge instructions. By putting our heads together in all these areas, we maintain remarkable consistency. The staff and the patients know what to expect. This reduces variability and increases the likelihood that we’ll execute a joint procedure without problems.”
To be more efficient, Dr. Dare pared down his tray to only what he needs for TSAs. He uses the same retractors and other tools for every case, which makes things easier for him, the scrub tech and the sterile processing staff. Everything fits on one mayo stand next to him.
Anesthesia and patient selection
A team proficient in performing regional blocks is by far the most important component of a successful outpatient shoulder program, says J. Gabriel Horneff III, MD, FAAOS, assistant professor of clinical orthopedic surgery in the shoulder and elbow division at University of Pennsylvania in Philadelphia. Anesthesiologists must also be willing to properly explain what patients should expect from the blocks so they don’t think a normal side effect such as numbness of the arm or the short-term lack of ability to use the arm is a serious complication. They also must check in on patients, not just wait for them to call if something is wrong.
Your team should know how to stratify which patients can have their shoulders replaced in an ASC or a hospital. Get clearance from a cardiologist or order a more extensive cardiac workup to make sure it’s safe to send a patient home. The best candidates for outpatient shoulders have healthy BMIs and no comorbidities such as congestive heart failure, COPD, immunodeficiencies or severe shoulder deformities.
Patients were in the hospital for up to a week after a shoulder replacement only 10 years ago. Now we know that these patients are at less risk for blood clots, infections and other perioperative complications if they’re at home. Knee and hip replacements led the charge into the outpatient arena, but outpatient shoulders are taking place at a higher rate than their predecessors and could soon be the fastest-growing service line in many orthopedic practices. OSM
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)