- Home
- The Magazine
- Article
OR Excellence Awards: Employee Engagement & Safety: Pride, Passion and Performance Improvement
By: Joe Paone | Senior Editor
Published: 9/5/2024
After an employee engagement survey raised red flags, leadership and staff at The Ambulatory Surgical Pavilion at Robert Wood Johnson University Hospital collaborated to address the issues.
With more than 30 staff members and numerous physicians performing thousands of surgeries in various specialties, it was difficult to get everyone on the same page at The Ambulatory Surgical Pavilion (ASP) at Robert Wood Johnson University Hospital in New Brunswick, N.J. A culture of open communication and collaboration was lacking. Two years later, the difference is obvious both anecdotally and through various performance metrics. As a result, the ASP is our 2024 OR Excellence Award winner in the category of Employee Engagement & Safety.
‘Survey says…’
To improve employees’ experience and better understand their needs and concerns, ASP conducts an annual employee engagement survey. Rowena Lim, DNP, MBA, RN, director of patient care, says it measures employees’ degree of pride in the organization, intention to stay, willingness to recommend and satisfaction.
In 2022, the survey generated an 81% response rate and raised red flags with unfavorable results in three areas: effective teamwork between nurses and physicians; event reporting focused on solving problems rather than write-ups, and efficient communication between physicians, nurses and support services. Each area, says Dr. Lim, needed to be addressed to promote a positive, healthy, collaborative work environment and build high-performance teams.
The results were shared and discussed in a staff meeting. Dr. Lim says this was a turning point, as staff gained a greater trust for leadership. “When the staff realized their leaders are there to help them and work through processes with them, they became more vocal,” she says. The nature of daily conversations between leaders and staff changed, particularly about things that needed fixing or improvement. “When we talk about a problem, it’s like, ‘OK, let’s make a plan. What can we do better? How can we do it better?’”
Everyone was asked to think about the survey results and develop solutions — and did they ever!
• Teamwork. Nursing leaders collaborated with human resources to develop two-hour teambuilding courses focused on increasing trust and respect and building strong working relationships. The well-attended, well-received program, administered in June and July 2023, focused on improving team dynamics, setting ground rules and team expectations, fostering respectful communication and creating a positive work environment. An OR nurse volunteered to become the ASP’s Kindness Champion, leading the effort to create a more harmonious work environment.
• Community outreach. Developing pride led to doing good in the community. A charge nurse suggested a group outreach project to improve interpersonal relationships. Staff now participate in the Ronald McDonald House’s Adopt a Family program. For two consecutive years, the team has sponsored at least two families every Christmas.
• Communication. Nursing leaders placed a large visibility board in pre-op to improve communication throughout the unit. The “vis wall” includes vital daily stats such as case volume; number of ORs running; readiness of staffing, equipment, instruments and supplies; and metrics including first case on-time start, turnaround time and patient satisfaction scores. It also includes words about the site’s vision, mission, values and staff commitment.
“The vis wall is our unit’s story board of who we are, what we are and what we aspire to become,” says Dr. Lim, noting it often launches conversations about improvements. “What is lacking? What can we do together to reach this goal? Just talking at the team will not work. I am transparent and honest with them. By gaining their trust, we work together.”
• Event reporting. A “system safety together” campaign encourages staff to speak up to leaders. An icon on all computers in the unit provides an easy reporting mechanism for staff. Reported events go to respective leaders as well as the risk management and quality/safety departments for review and investigation, and are discussed in daily huddles to raise awareness. Leadership works with staff on improvements and closes the loop by reporting the courses of action that were put in place.
• Team engagement. ASP employees now participate in monthly hospital and unit committee meetings at a greater than 90% rate. They are empowered to work on performance improvement projects, and additionally benefit by using their committee affiliations and improvement projects for clinical ladder application. “We have greater than 60% CNOR certified and 100% surgical tech certified,” says Dr. Lim. “We have 90% BSNs with 10% registered in MSN programs.”
Proactivity and trust
If the 2022 employee engagement survey served as a wake-up call, the 2023 survey showed a facility that was awake and energized. Analysis showed significant improvements in teamwork, pride and reporting. “Employees feel well-equipped, and there’s effective communication and teamwork within and between departments,” says Dr. Lim. “They feel the organization places an emphasis on safety and would feel comfortable recommending it for patient care. They feel comfortable speaking up, and that mistakes are used as learning experiences.”
The results have been tangible in terms of both process improvement and team spirit. In 2023, for example, first case on-time starts rose by 24% and turnaround times declined from 24 to 22 minutes. “How can we improve? How can we attain that?” says Dr. Lim. “By working together.” OSM
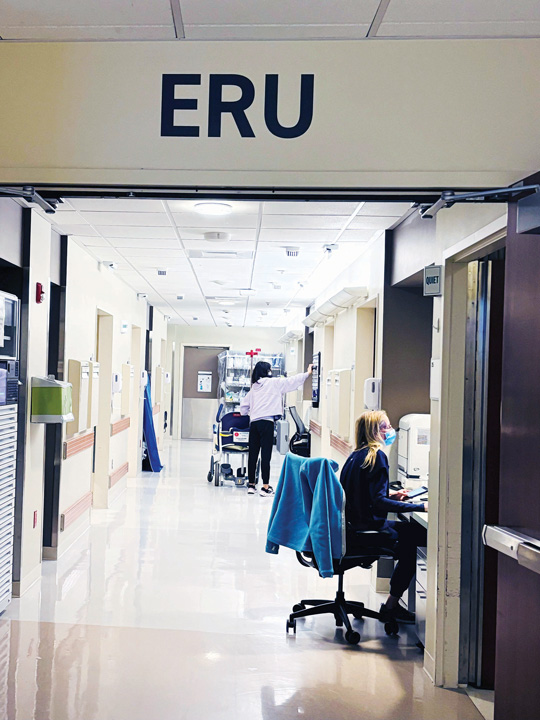
At Overlake Medical Center in Bellevue, Wash., recovering same-day orthopedic surgery patients were intermixed on an inpatient unit. With discharge often taking six hours, it cohorted the patients in a new extended recovery unit (ERU) in the perioperative area. The ERU provides a better patient experience, more specialized care and quicker access to physical therapy, while allowing the inpatient unit to focus on patients requiring acute care.
A collaborative effort from leaders and staff across various units and disciplines made it happen quickly. The team secured surgeon and executive approval to staff and equip six patient rooms. It engaged pharmacy to speed access to medications, physical therapy to arrive more quickly, and dietary services to provide nutritious food to recovering patients. Periop nurses trained ortho nurses on workflow. A group chat quickly addresses patient needs and transfers. Comparing 2020 to 2023, average time to post-op mobility declined from 3.3 to 1.2 hours, day-of-surgery PT evaluation rose from 89% to 95%, and length of stay dipped from 6.2 to 2.3 hours, while readmission and return to ED rates stayed virtually the same.
The success and safety of the ERU impressed surgeons so much that the cohort’s patient volume doubled. Staff enjoy working together in the new workflow and area. Patients note every team member they encounter seems to be on the same page. “It was a full symphony,” says Gordy Fields, MSN, RN, clinical manager of orthopedics and spine. — Joe Paone
.svg?sfvrsn=be606e78_3)
.svg?sfvrsn=56b2f850_5)